When opioids and benzodiazepines are taken together, the risk of stopping breathing doesn’t just go up-it explodes. This isn’t a theoretical concern. It’s happening every day in homes, clinics, and emergency rooms across the country. The FDA issued its first official warning in 2016, and by 2019, they strengthened it with a Boxed Warning-the highest level of alert-for both drug classes. Why? Because the numbers don’t lie: people who take both drugs are ten times more likely to die from an overdose than those taking opioids alone.
How These Drugs Kill Together
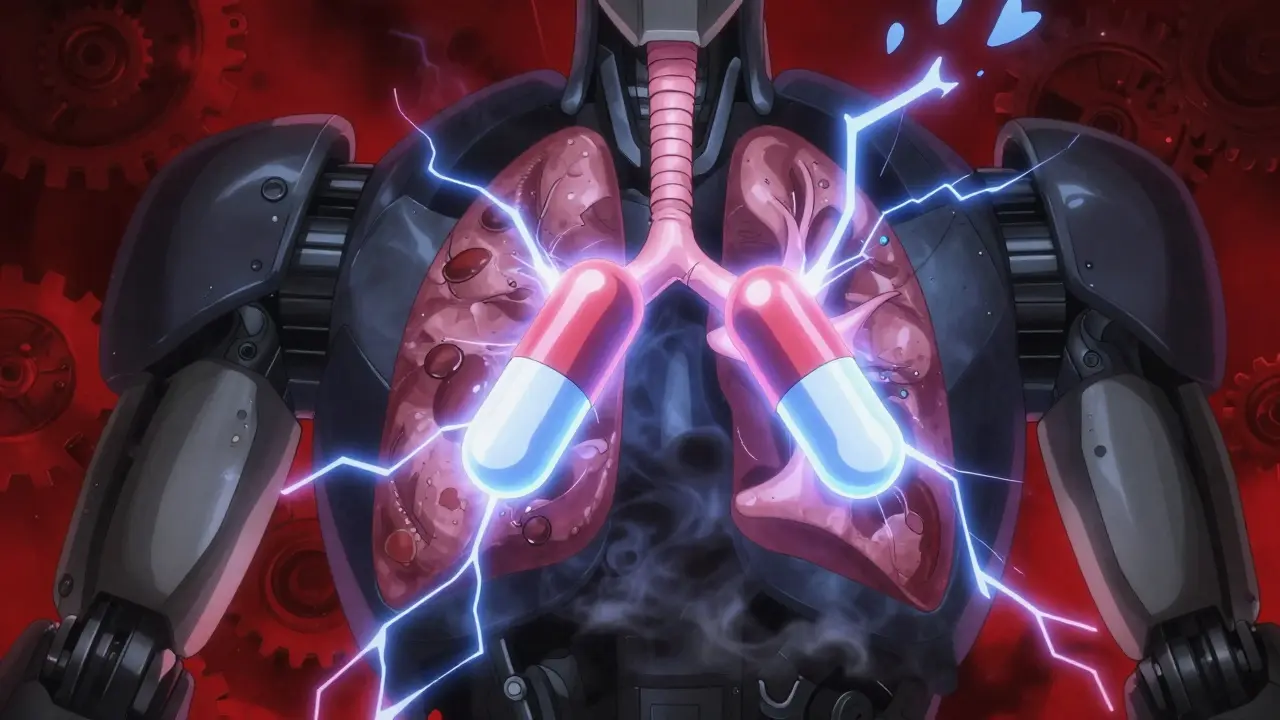
Opioids like oxycodone, fentanyl, and hydrocodone work by binding to mu-opioid receptors in the brainstem, the area that controls automatic breathing. Benzodiazepines like alprazolam, lorazepam, and diazepam boost the effect of GABA, a calming neurotransmitter that slows down nerve activity-including the signals that tell your lungs to breathe. Individually, each drug can cause drowsiness and shallow breathing. Together, they don’t just add up-they multiply.Studies show that when these drugs are combined, oxygen levels in the blood drop dramatically. One human trial found that 85% of participants taking both drugs had oxygen saturation fall below 90%, compared to only 45% taking opioids alone. That’s not just sleepy-it’s life-threatening. The brain’s ability to respond to rising carbon dioxide levels, which normally triggers deeper breathing, becomes severely blunted. Even people who’ve been on opioids for years and think they’ve built up tolerance aren’t protected. Their bodies haven’t adapted to benzodiazepines’ effect on breathing.
There’s another hidden danger: drug metabolism. Some opioids, including fentanyl and methadone, are broken down by the liver enzyme CYP3A4. Benzodiazepines like alprazolam and ketoconazole can block this enzyme. That means the opioid stays in the body longer, building up to toxic levels even if the dose hasn’t changed. A person might be taking their usual pain pill, add a sleeping pill, and suddenly find themselves in respiratory arrest-without realizing why.
Who’s Most at Risk?
It’s not just people using drugs recreationally. Many of those at highest risk are patients prescribed both medications by doctors. Older adults are especially vulnerable. The American Geriatrics Society lists this combination as potentially inappropriate for seniors in their Beers Criteria, citing increased fall risk and respiratory depression. People with sleep apnea, COPD, or other lung conditions face even greater danger. The combination can turn mild snoring into full-blown airway collapse.Even patients on opioid replacement therapy for addiction-like those on methadone or buprenorphine-are at risk. Their tolerance to opioids doesn’t extend to benzodiazepines. A 2021 review in the Annals of Palliative Medicine found that clinicians often mistakenly assume these patients can handle higher sedative doses, leading to fatal miscalculations.
Emergency room data shows that 16% of opioid-related overdose deaths in 2020 involved benzodiazepines. That’s roughly 30% of all opioid overdoses. The CDC reported that the death rate from this combination rose from 0.6 per 100,000 in 1999 to 8.8 per 100,000 in 2017. While it’s dipped slightly since, it’s still far above historical levels.
What Happens During an Overdose?
The signs don’t always look like a typical overdose. There’s no screaming, no thrashing. Often, it’s quiet. The person becomes extremely drowsy, slurs their words, or can’t stay awake. Their breathing slows to just a few breaths per minute-shallow, irregular, and ineffective. Lips or fingertips turn blue. They may nod off and not wake up. In many cases, family members find them unresponsive hours later, thinking they were just sleeping deeply.What makes this so dangerous is how easily it can be missed. A person might seem fine during a doctor’s visit. Their oxygen levels might look okay on a pulse oximeter. But that device doesn’t detect the slow, silent decline that happens during sleep. That’s when the combination becomes lethal. The brain stops responding to rising CO2. The airway collapses. Breathing stops. And there’s no alarm.
Doctors Are Being Warned-But It’s Still Happening
The FDA, CDC, and major medical societies all agree: avoid prescribing these drugs together unless absolutely necessary. The CDC’s 2022 opioid prescribing guidelines say to avoid benzodiazepines with opioids whenever possible. The FDA says if you must prescribe both, start with the lowest possible dose of the benzodiazepine and monitor closely.Yet, a 2021 study in JAMA Network Open found that 15% of Medicare Part D patients on long-term opioids were also getting benzodiazepines. In 4.3% of cases, it was a high-risk combo-extended-release opioids with long-acting benzos. That’s tens of thousands of people still being exposed to this deadly mix.
Some healthcare systems are fighting back. Electronic health records now include automated alerts that pop up when a prescriber tries to write both scripts. One study showed these alerts reduced dangerous co-prescribing by 27.3%. But alerts aren’t foolproof. If a doctor clicks past them, the system can’t stop the prescription.
What Should You Do If You’re Taking Both?
If you’re on both medications, don’t stop suddenly. Withdrawal from benzodiazepines can trigger seizures. Opioid withdrawal is brutal-sweating, vomiting, anxiety, rapid heartbeat. Abruptly quitting either one can be dangerous. But continuing both? That’s a death sentence waiting to happen.Here’s what to do:
- Call your doctor. Don’t wait for your next appointment. Tell them you’re concerned about the risks.
- Ask if there’s a safer alternative. For anxiety, consider therapy, SSRIs, or non-benzodiazepine sleep aids. For pain, explore physical therapy, nerve blocks, or non-opioid medications like gabapentin or acetaminophen.
- If you must continue both, never take them together without supervision. Avoid alcohol, sleep aids, or any other sedatives.
- Have naloxone on hand. It won’t reverse benzodiazepine effects, but it can help if opioids are part of the overdose. Make sure someone you live with knows how to use it.
- Use a pulse oximeter at home if you’re at high risk. If your oxygen drops below 92% for more than a few minutes, seek help immediately.
The Bottom Line
This isn’t about being careful. It’s about avoiding the combination entirely. The science is clear. The deaths are real. The warnings have been out for years. Yet people are still dying because they didn’t know, or because they were told it was safe.If you’re prescribed both, ask: Is this truly necessary? Is there another way? And if you’re a caregiver, watch for signs: Is your loved one harder to wake? Are they unusually confused or slow to respond? Don’t assume they’re just tired. It could be the beginning of the end.
One drug can be managed. Two together? That’s a recipe for disaster. The system has failed too many people already. Don’t let it fail you.
Jess Bevis
January 27, 2026 AT 14:57This combo kills quietly. No drama, no warning. Just stops breathing while they sleep.
Robert Cardoso
January 29, 2026 AT 10:11Let’s be clear: this isn’t a ‘risk’-it’s a predictable pharmacological suicide pact. Opioids depress the brainstem’s respiratory center; benzos suppress the cortical and limbic override that might otherwise compensate. Together, they disable every backup system the body has. The 10x mortality increase? That’s conservative. Studies like the one in JAMA Internal Medicine (2020) show that when you combine long-acting benzos with fentanyl analogs, the median time to respiratory arrest drops to 47 minutes post-ingestion. And no, tolerance doesn’t protect you-your mu-receptor downregulation doesn’t extend to GABAergic suppression. The liver enzyme inhibition? CYP3A4 blockade by alprazolam and ketoconazole creates a perfect storm for opioid accumulation. This isn’t negligence-it’s systemic malpractice disguised as treatment.
Anna Lou Chen
January 29, 2026 AT 19:46It’s the ultimate irony of modern medicine: we weaponize neurochemical tranquility to treat anxiety, then weaponize it again to kill the very people we claim to help. The pharmaceutical-industrial complex doesn’t care about your breath-it cares about your refill rate. We’ve turned the human nervous system into a profit margin. And now we’re surprised when the wires short-circuit? The Beers Criteria exists for a reason. Yet doctors still write these scripts like they’re handing out candy at Halloween. Where’s the accountability? Where’s the moral courage? Or are we all just complicit in this slow-motion euthanasia?
fiona vaz
January 30, 2026 AT 21:39I’ve seen this firsthand with my dad. He was on oxycodone for back pain and lorazepam for sleep after his surgery. One night, he didn’t wake up. We thought he was just exhausted. Turned out his O2 was at 78%. He’s fine now-after a long rehab-but I’ll never forget how quietly it happened. Please, if you’re on both, talk to your doctor. There are safer options. You’re not weak for asking.
Sue Latham
February 1, 2026 AT 11:49OMG I can’t believe people are still doing this?? Like… are you trying to die?? 😒 I had a friend who took Xanax with her pain meds and woke up in the ER with her boyfriend screaming. Like… just don’t? I know it’s hard but… there’s therapy. And yoga. And CBD. Like… pick one thing that doesn’t make you stop breathing??
John Rose
February 2, 2026 AT 15:17While the data is unequivocal, I’m curious about the clinical context. Are there any peer-reviewed studies that examine the risk-benefit ratio in palliative care settings where both drugs are used for refractory symptoms? The FDA warnings are critical, but in end-of-life scenarios, the goal isn’t always longevity-it’s comfort. Could there be a nuanced argument for carefully monitored co-prescribing in specific contexts, even if it’s statistically dangerous?
Lexi Karuzis
February 2, 2026 AT 20:06THEY’RE DOING THIS ON PURPOSE!! THE FDA, THE PHARMA COMPANIES, THE DOCTORS-THEY ALL KNOW THIS KILLS PEOPLE, BUT THEY KEEP DOING IT BECAUSE THEY MAKE BILLIONS OFF THE OVERDOSING!! I READ A LEAKED EMAIL FROM PFEIZER WHERE THEY SAID ‘THEY’LL DIE ANYWAY, SO WHY NOT MAKE A PROFIT?’ AND THE CDC? THEY’RE COVERING IT UP!! MY COUSIN DIED IN 2018-THEY SAID ‘ACCIDENTAL OVERDOSE’-BUT I KNOW THEY GAVE HIM BOTH!! THEY WANT US WEAK!! THEY WANT US DEPENDENT!! I’M NOT TAKING ANYTHING NOW!! I’M ON A RAW FOOD DIET AND ONLY BREATHING THROUGH MY NOSE!!
Colin Pierce
February 3, 2026 AT 17:15My brother was on methadone for years after his injury. He started taking diazepam for insomnia after his mom passed. He never thought it was a big deal-he’d been on opioids forever. He didn’t know his body hadn’t adapted to the benzo’s effect on breathing. He died in his sleep. I didn’t know until the coroner called. I wish someone had sat us down and said, ‘This combo is a silent killer.’ Please, if you’re reading this and you’re on both-don’t wait. Talk to someone. Even if you think you’re fine. You’re not.
Lance Long
February 4, 2026 AT 23:30I know how hard it is to come off these meds. I’ve been there. But you’re not alone. I was on oxycodone and clonazepam for three years after my accident. My doctor kept saying, ‘It’s fine, you’re stable.’ But I felt like I was walking through molasses. One day, I couldn’t get out of bed. That’s when I asked for help. We tapered slowly-over six months. I started therapy, got a sleep study, switched to gabapentin. It wasn’t easy. But I’m breathing again. And I’m alive. You can do this. One step at a time. You’ve already taken the hardest one-by reading this.
Brittany Fiddes
February 6, 2026 AT 19:17Of course this is happening-America’s entire healthcare system is a capitalist dumpster fire. Meanwhile, in the UK, we have NICE guidelines that outright ban this combination for anyone over 65. We don’t have this problem because we don’t treat medicine like a fast-food menu. Your doctors are incentivized to prescribe, not to protect. You’re being sold a death sentence wrapped in a prescription bottle. And you wonder why we think Americans are reckless? It’s not the people-it’s the system. Fix the system, not just the patient.
Mark Alan
February 7, 2026 AT 08:25💀 THIS IS WHY WE NEED NALOXONE IN EVERY HOME. Like, seriously. I keep two in my glovebox and one by my bed. My cousin used to take Xanax with his pain meds. One night, he didn’t wake up. His roommate used naloxone, called 911, and he survived. But he’s not the same. He has brain damage. Don’t wait for the worst to happen. Get the nasal spray. Teach your family how to use it. It’s free at most pharmacies. Just do it. 💪
James Dwyer
February 8, 2026 AT 04:13I was skeptical at first-thought it was just fear-mongering. But after reading the CDC stats and seeing how many people I know who’ve lost loved ones this way… I can’t unsee it. I talked to my doctor last week. We’re cutting the benzo out and trying CBT for my anxiety. It’s scary, but I’d rather be anxious and alive than peaceful and gone. Thanks for the wake-up call, post. Needed this.