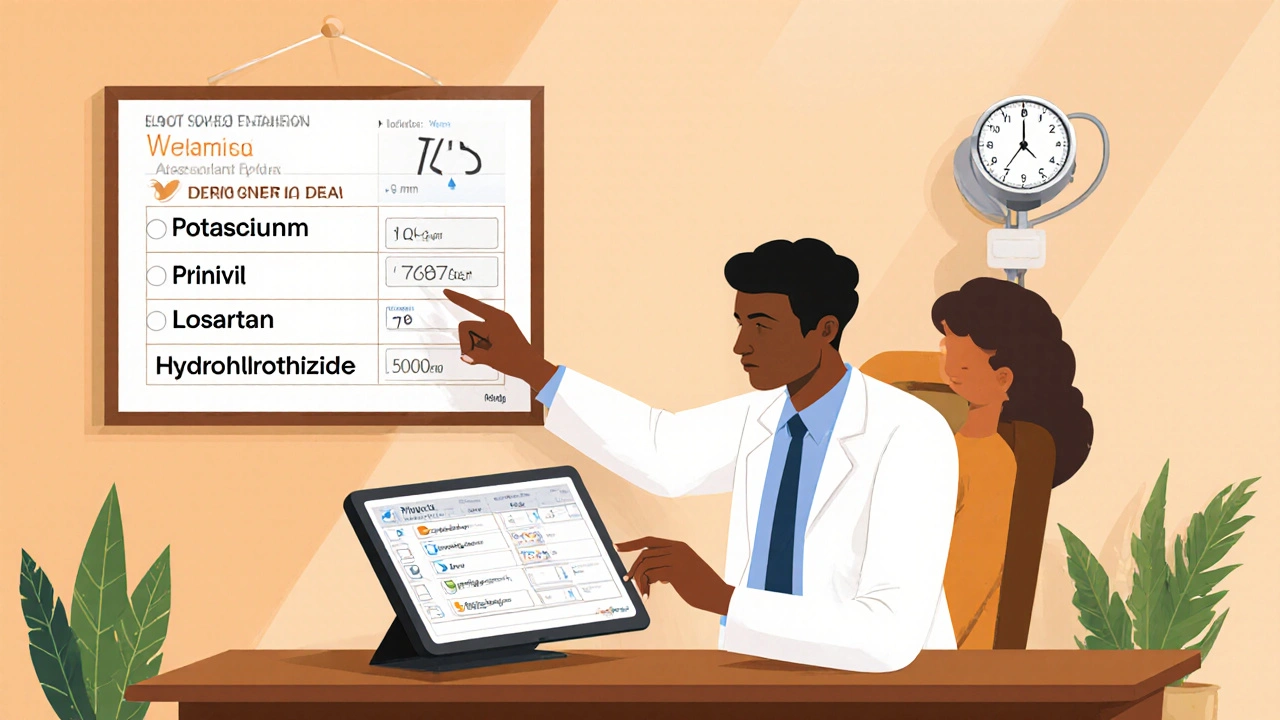
Blood Pressure Medication Selector
Recommended Medication:
Key Considerations:
When it comes to controlling high blood pressure, the market is crowded with pills that promise the same outcome. Picking the right one means understanding how each drug works, its side‑effect profile, and where it fits into your health picture. Below you’ll find a side‑by‑side look at Prinivil is the brand name for lisinopril, an ACE inhibitor used to treat hypertension and heart failure and the most common alternatives, so you can decide which matches your needs.
Quick Takeaways
- Prinivil (lisinopril) blocks the enzyme that narrows blood vessels, lowering pressure in most patients.
- ACE inhibitors often cause a persistent dry cough; ARBs such as losartan avoid this.
- Cost differences are narrowing-generic lisinopril averages $4 per month, while many generics of alternatives sit between $2‑$8.
- Kidney function and potassium levels are key labs when choosing between ACE inhibitors and ARBs.
- Combination therapy (e.g., ACE inhibitor+thiazide diuretic) is common for resistant hypertension.
What Is Prinivil (Lisinopril)?
Lisinopril belongs to the class of ACE inhibitors. It works by inhibiting the angiotensin‑converting enzyme, which reduces the production of angiotensinII, a molecule that tightens arteries. With less angiotensinII, blood vessels relax, blood pressure drops, and the heart’s workload eases. The typical starting dose for adults with hypertension is 10mg once daily, titrated up to 40mg if needed. Common side effects include a dry cough, elevated potassium, and occasional dizziness.
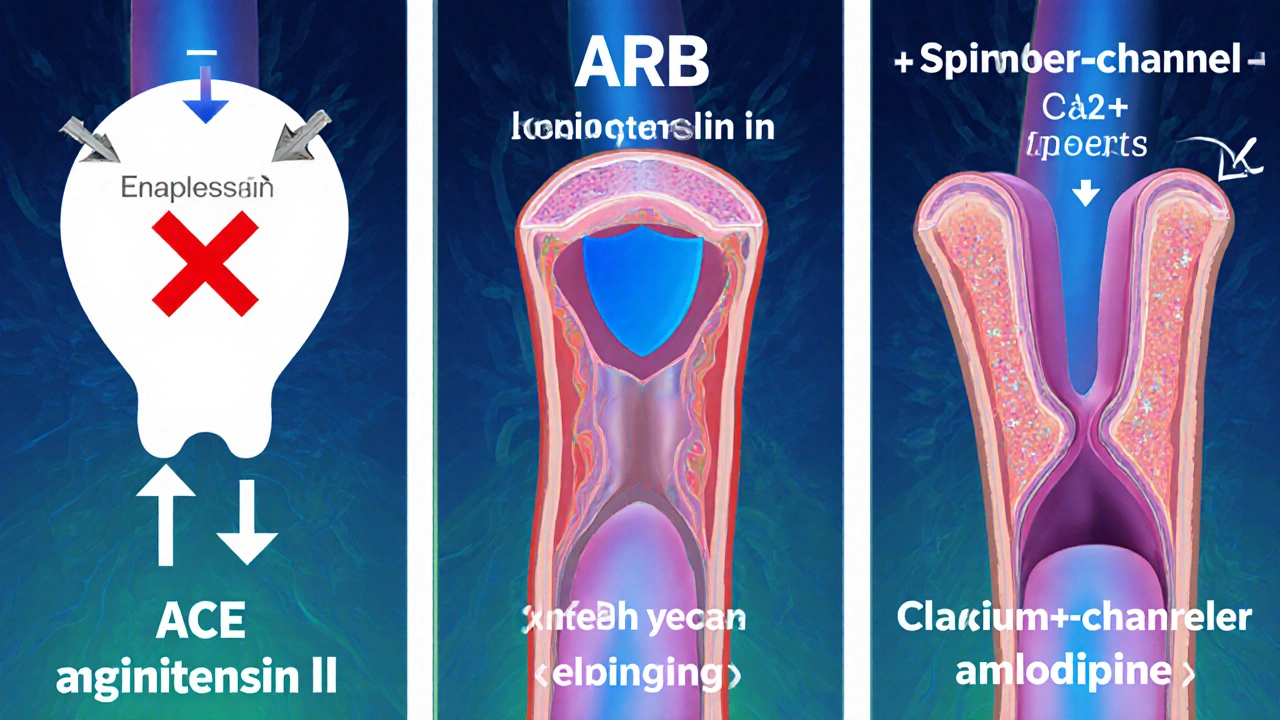
How ACE Inhibitors Differ From Other Classes
ACE inhibitors share a mechanism: they block the conversion of angiotensinI to angiotensinII. In contrast, ARBs (angiotensinII receptor blockers) prevent angiotensinII from binding to its receptors, offering a similar pressure‑lowering effect without the cough trigger. Calcium‑channel blockers like Amlodipine relax the smooth muscle directly, while thiazide diuretics such as Hydrochlorothiazide reduce fluid volume.
Popular Alternatives to Prinivil
Enalapril
Enalapril is another ACE inhibitor, often prescribed at 5‑20mg daily. It has a similar cough risk but may be better for patients with mild renal impairment because it is metabolized to an active form in the liver.
Losartan
Losartan belongs to the ARB family. Starting doses range from 50‑100mg once daily. Losartan is the go‑to when a patient can’t tolerate the ACE‑inhibitor cough, and it demonstrates comparable blood‑pressure control in most trials.
Valsartan
Valsartan is another ARB, usually dosed at 80‑320mg per day. It tends to have a slightly lower cost than losartan and shows a modest benefit for patients with heart failure.
Ramipril
Ramipril is an ACE inhibitor with a longer half‑life, allowing once‑daily dosing of 2.5‑10mg. Studies suggest it may lower the risk of cardiovascular events more effectively than some newer ACE inhibitors.
Amlodipine
Amlodipine is a calcium‑channel blocker, typically started at 5mg daily. It’s especially useful for patients with isolated systolic hypertension or peripheral artery disease.
Hydrochlorothiazide
Hydrochlorothiazide (HCTZ) is a thiazide diuretic, dosed 12.5‑50mg daily. It works by increasing urine output, lowering blood volume. Frequently combined with an ACE inhibitor or ARB for additive effect.
Comparison at a Glance
| Drug (generic) | Class | Typical daily dose | Mechanism | Average monthly cost (US) | Common side effects |
|---|---|---|---|---|---|
| Lisinopril | ACE inhibitor | 10‑40mg | Blocks ACE → ↓ AngiotensinII | $4 | Cough, hyperkalaemia, dizziness |
| Enalapril | ACE inhibitor | 5‑20mg | Blocks ACE → ↓ AngiotensinII | $5 | Cough, rash, elevated creatinine |
| Losartan | ARB | 50‑100mg | Blocks AT1 receptor → ↓ AngiotensinII effect | $6 | Dizziness, hyperkalaemia, rare liver issues |
| Valsartan | ARB | 80‑320mg | Blocks AT1 receptor → ↓ AngiotensinII effect | $5 | Headache, fatigue, hyperkalaemia |
| Ramipril | ACE inhibitor | 2.5‑10mg | Blocks ACE → ↓ AngiotensinII | $5 | Cough, dry mouth, angio‑edema |
| Amlodipine | Calcium‑channel blocker | 5‑10mg | Inhibits Ca²⁺ entry → vasodilation | $7 | Peripheral edema, flushing, gum hyperplasia |
| Hydrochlorothiazide | Thiazide diuretic | 12.5‑50mg | Increases Na⁺/Cl⁻ excretion → ↓ plasma volume | $3 | Electrolyte loss, photosensitivity, gout flare |
Decision Criteria: How to Choose the Right Drug
Below are the top factors clinicians weigh when picking a therapy:
- Renal function: ACE inhibitors and ARBs can raise serum creatinine; if eGFR <30mL/min/1.73m², a lower starting dose or an alternative like amlodipine is safer.
- Cough risk: A persistent dry cough points to ACE inhibition. Switching to an ARB (losartan or valsartan) resolves this in >80% of patients.
- Potassium levels: Both ACE inhibitors and ARBs can cause hyperkalaemia, especially when combined with potassium‑sparing diuretics.
- Cost & insurance coverage: Generic lisinopril, enalapril, and HCTZ have the lowest out‑of‑pocket prices; newer ARBs may be tier‑2 or tier‑3.
- Comorbid conditions: Heart failure benefits are strongest with ACE inhibitors or ARBs; diabetes with microalbuminuria often leans toward ACE inhibition.
- Medication burden: Once‑daily dosing improves adherence. Lisinopril, enalapril, ramipril, and amlodipine all fit this profile.
Best‑Fit Scenarios for Each Option
| Drug | Ideal Patient Profile |
|---|---|
| Prinivil (Lisinopril) | Newly diagnosed hypertension, good kidney function, no prior cough, cost‑sensitive. |
| Enalapril | Patients needing a lower‑dose ACE inhibitor, mild liver disease (active metabolite). |
| Losartan | Patients who developed ACE‑inhibitor cough, African‑American patients (often better response). |
| Valsartan | Heart failure with reduced ejection fraction needing ARB’s proven mortality benefit. |
| Ramipril | Patients with high cardiovascular risk where long‑term outcome data favor ramipril. |
| Amlodipine | Isolated systolic hypertension, peripheral artery disease, or when edema is manageable. |
| Hydrochlorothiazide | Stage‑1 hypertension, especially when a diuretic‑first approach is recommended. |
Common Pitfalls & How to Avoid Them
- Skipping baseline labs: Always check creatinine and potassium before starting an ACE inhibitor or ARB.
- Ignoring drug interactions: NSAIDs can blunt the antihypertensive effect and worsen kidney function when combined with ACE inhibitors.
- Under‑dosing: Starting too low and never titrating may leave patients uncontrolled. Aim for target BP <130/80mmHg in most adults.
- Not addressing cough early: A persistent cough after two weeks often signals ACE inhibition; switch to an ARB before patient stops medication.
- Overlooking adherence: Once‑daily pills like lisinopril improve compliance. Use pill organizers or refill reminders.
Frequently Asked Questions
Can I take Prinivil with a thiazide diuretic?
Yes. Combining an ACE inhibitor like lisinopril with a thiazide diuretic (e.g., hydrochlorothiazide) is a common strategy for patients whose blood pressure remains high on a single drug. The duo works synergistically, but monitor potassium and kidney function closely.
Why do some people develop a cough on ACE inhibitors?
ACE inhibitors block the breakdown of bradykinin, a peptide that can irritate the airway lining, leading to a dry, persistent cough. Switching to an ARB eliminates this pathway, so the cough usually disappears.
Is lisinopril safe during pregnancy?
No. ACE inhibitors are classified as pregnancy category D and have been linked to fetal kidney problems, low amniotic fluid, and even birth defects. Women of child‑bearing age should use effective contraception or discuss safer alternatives like labetalol.
How quickly does blood pressure drop after the first dose?
Lisinopril begins to lower systolic pressure within 4‑6hours, reaching peak effect around 6‑8hours. Full steady‑state control may require 2‑4 weeks of consistent dosing.
Can I switch from Prinivil to losartan without a washout period?
A direct switch is generally safe because both drugs affect the renin‑angiotensin system. However, clinicians often wait 24‑48hours to monitor blood pressure and potassium, especially if the patient has kidney disease.
Next Steps
1. Review your recent labs (creatinine, eGFR, potassium).
2. Match your health profile against the decision criteria above.
3. Discuss with your prescriber whether a single agent (Prinivil) suffices or if a combination/alternative better fits your situation.
4. If you experience a cough, schedule a quick appointment to consider an ARB swap.
5. Use a medication tracker app to keep doses consistent and set refill reminders.
Choosing the right antihypertensive isn’t a one‑size‑fits‑all decision. By understanding each drug’s strengths, side‑effect footprint, and cost, you can partner with your healthcare team to land on the therapy that keeps your blood pressure down and your quality of life up.


Hope Reader
October 8, 2025 AT 13:12So you’re stuck picking a pill, huh? Here’s the quick cheat sheet: lisinopril is cheap, works for most, but watch for that dry cough ;)
If your kidneys are fine and potassium is normal, it’s often the first‑line choice.
Got a history of cough with ACE inhibitors? Switch to an ARB like losartan and you’ll sleep better.
When cost matters, generic lisinopril is usually around four bucks a month, which beats many branded ARBs.
And remember to check creatinine and potassium before you start – those labs are the gatekeepers.
Marry coral
October 9, 2025 AT 11:25Listen, if you can’t tolerate a cough just drop the ACE and grab an ARB. It’s not rocket science, it’s basic patient care.
Emer Kirk
October 10, 2025 AT 09:05i love how everybody thinks a pill will solve everything i mean sure it lowers pressure but what about diet exercise and stress really you need a whole plan not just a bottle of stuff
Roberta Saettone
October 11, 2025 AT 06:45Alright, let’s dig into why the “one‑size‑fits‑all” approach to hypertension medication can be misleading. First, ACE inhibitors like lisinopril are fantastic for patients with heart failure or diabetic nephropathy because they reduce proteinuria and improve survival. Second, the dreaded dry cough isn’t just a nuisance; it can lead to non‑adherence, so swapping to an ARB such as losartan or valsartan is often the logical next step. Third, kidney function matters – an eGFR below 30 mL/min nudges clinicians toward diuretics or calcium‑channel blockers because ACE inhibitors and ARBs can elevate creatinine. Fourth, hyperkalaemia is a real risk when you combine ACE inhibitors or ARBs with potassium‑sparing diuretics or supplements, so regular labs are non‑negotiable. Fifth, cost is a driver of choice; generic lisinopril hovers around $4 per month, while some ARBs sit at $6‑$8, though insurance formularies can flip the equation. Sixth, combination therapy – think ACE inhibitor plus thiazide – is a common strategy for resistant hypertension, but you still need to monitor electrolytes. Seventh, patient ethnicity can influence response; African‑American patients often achieve better blood pressure control with calcium‑channel blockers or thiazides. Eighth, comorbid gout pushes you away from thiazides because they can raise uric acid levels. Ninth, the once‑daily dosing of lisinopril, ramipril, and amlodipine improves adherence, especially in older adults. Tenth, drug interactions matter – NSAIDs blunt the antihypertensive effect and can worsen renal function when paired with ACE inhibitors. Eleventh, lifestyle modifications remain the foundation: reduced sodium, weight loss, regular aerobic exercise, and limiting alcohol. Twelfth, patient preference is key; many will choose the medication with the fewest side effects, even if it costs a bit more. Thirteenth, you should never start an ACE inhibitor without a baseline potassium and creatinine check. Fourteenth, if a patient is already on a potassium‑sparing diuretic, consider an ARB over an ACE inhibitor to minimize cough risk. Fifteenth, always educate patients about the signs of angio‑edema – swelling of the lips or tongue is a medical emergency. Sixteenth, follow‑up within two weeks of initiating therapy to assess blood pressure response and tolerability. By keeping these nuances in mind, you can tailor therapy rather than just slap a pill on the chart.
Sue Berrymore
October 12, 2025 AT 04:25Let’s get pumped about taking control of your BP! 🎉 You’ve got options, so pick the one that fits your life. If you’re over 65, once‑daily dosing is a lifesaver for sticking to the plan. Got a cough? Dump the ACE and grab an ARB – you’ll thank yourself later. And don’t forget to pair any drug with diet tweaks; sodium isn’t your friend. Keep those labs in check and you’ll breeze through the hypertension marathon.
Jeffrey Lee
October 13, 2025 AT 02:05Ok so i guess the cheap stuff works but u know thers a bunch of new generics that are just as good? also i think the article missed the fact that some people cant take ACE at all because of... maybe i dont know i just read somewhere that the blood pressure can actually go crazy if you mix with certain supplements lol
Ian Parkin
October 13, 2025 AT 23:45Dear reader, I respectfully encourage you to consider the comprehensive clinical guidelines when selecting an antihypertensive agent. It is paramount to evaluate renal function, serum potassium, and any coexistent comorbidities, such as heart failure or diabetes mellitus, prior to commencing therapy. Moreover, cost‑effectiveness analyses frequently demonstrate that generic lisinopril remains a judicious first‑line option for the majority of patients, provided no contraindications exist. Should an adverse cough develop, an angiotensin‑II receptor blocker may be substituted without compromising therapeutic efficacy. I trust this clarification proves beneficial.
Julia Odom
October 14, 2025 AT 21:25In a formal sense, the evidence supports that ACE inhibitors such as lisinopril confer mortality benefit in individuals with established cardiovascular disease. Nevertheless, the practical discourse must also acknowledge patient preferences and potential side‑effects, notably cough. Transitioning to an ARB is a legitimate strategy when tolerability is compromised. A balanced approach that integrates pharmacologic efficacy with individual circumstance is advisable.
Danielle Knox
October 15, 2025 AT 19:05Well, isn’t this just another glorified drug catalog? If you want the cheapest pill, just grab the generic. If you’re allergic to cough, pick an ARB – you’re welcome for the obvious advice.
Mark Evans
October 16, 2025 AT 16:45Seriously, the best choice is the one you’ll actually take. If a cheap ACE works for you and you don’t mind the occasional dry cough, stick with it. If the cough drives you nuts, switch to an ARB – it’s a simple trade‑off. Bottom line: pick the drug that fits your lifestyle and keep the labs in check.
Megan C.
October 17, 2025 AT 14:25Let me be perfectly clear: prescribing the wrong antihypertensive is a moral failing. If a patient can’t tolerate a cough, the physician has an ethical duty to change the regimen immediately. Ignoring hyperkalaemia risks is simply negligent. Do your job.
Greg McKinney
October 18, 2025 AT 12:05Oh sure, another ‘cheat sheet’ for the masses. As if we need another one‑size‑fits‑all list. People are individuals, not spreadsheet rows.
Dawna Rand
October 19, 2025 AT 09:45💡 Quick tip: always double‑check potassium before starting any ACE or ARB. It can save you a hospital visit later! 🌟
Effie Chen
October 20, 2025 AT 07:25🔎 Curious about why ARBs don’t cause cough? They block the receptor downstream, so the bradykinin build‑up that triggers the cough never happens. Pretty neat, right?
rohit kulkarni
October 21, 2025 AT 05:05Consider, if you will, the philosophical interplay between pharmacodynamics and the patient’s lived experience; indeed, the medication is but a vessel for the body’s own regulatory mechanisms-yet we must remain ever vigilant, for the iatrogenic shadows of hyperkalaemia loom large whenever we meddle with the renin‑angiotensin‑aldosterone system!; therefore, the prudent clinician embraces routine laboratory surveillance.
RONEY AHAMED
October 22, 2025 AT 02:45Just drop the ACE if you get a cough and pick an ARB. Easy as that.
emma but call me ulfi
October 23, 2025 AT 00:25Honestly, the best drug is the one you remember to take. Keep it simple.
George Gritzalas
October 23, 2025 AT 22:05Grammar Police alert: “Lisinopril” isn’t “lisinopril” in a title, folks. Also, if you’re going to brag about a “cheat sheet,” make sure the sheet actually answers the questions; otherwise, it’s just clutter. And please, stop treating every side‑effect like a death sentence – most patients tolerate a mild cough just fine.
Alyssa Matarum
October 24, 2025 AT 19:45Pick a drug, check labs, stay consistent.