When your spinal cord is injured, it’s not just about losing movement or feeling. It’s about relearning how to live. A spinal cord injury (SCI) doesn’t just break a nerve-it rewires your entire relationship with your body. Every day, around 49 people in the U.S. face this reality. Most are hit by car crashes, falls, or violence. And while the damage to the spinal cord itself can’t yet be fully repaired, what happens after the injury is where real change begins.
What Happens When the Spinal Cord Is Damaged
The spinal cord is your body’s main information highway. Signals from your brain travel down it to tell your muscles when to move, your bladder when to empty, and your skin when it’s hot or cold. When that highway is damaged, those signals get blocked. The higher the injury, the more functions are lost. A C1-C4 injury means you might not be able to breathe on your own. You’ll need help with turning your head, lifting your arms, or even swallowing. At C5-C6, you might keep shoulder and elbow movement but lose hand function. Below T1, you’re more likely to keep full arm use but lose leg control. Complete injuries mean no sensation or movement below the injury. Incomplete injuries mean some signals still get through-and that’s where recovery has the most room to grow. The good news? Your body doesn’t just sit still after injury. It adapts. Nerves rewire. Muscles learn to work differently. With the right rehab, people with incomplete injuries can regain 80-90% of their function within the first year. That’s not magic. It’s science.Rehab Starts the Day You’re Stabilized
Too many people think rehab begins when they leave the hospital. It doesn’t. It starts within 24 to 72 hours after the injury, even while you’re still in intensive care. The goal? Keep your body from falling apart while you heal. Early rehab is about preventing the secondary disasters that come after the initial trauma. Muscles turn stiff. Joints lock up. Lungs fill with fluid. Pressure sores form. That’s why therapists start moving you-even if you can’t move yourself. Passive range-of-motion exercises are done daily, sometimes three times a day, to keep your shoulders, elbows, and hips from freezing. Breathing is another big focus, especially for injuries at C3-C5. Assisted coughing, chest percussion, and incentive spirometry cut pneumonia risk by 65%. These aren’t optional. They’re lifesaving. Inpatient rehab programs run five days a week, with at least three hours of therapy daily. You’ll work with a team: physical therapists, occupational therapists, nurses, social workers, psychologists, and speech therapists. Everyone has a role. One person teaches you how to transfer from bed to wheelchair. Another helps you relearn how to dress yourself with one hand. A third helps you cope with the grief, anger, or fear that comes with losing control of your body.The Tools That Bring Back Function
Modern rehab isn’t just about stretching and strength. It’s about using technology to rebuild what’s broken. Functional Electrical Stimulation (FES) sends tiny electrical pulses to paralyzed muscles, making them contract. FES bikes let people with paraplegia pedal with their legs. Studies show this boosts heart health-increasing oxygen use by 14.3%, compared to just 5.2% with arm cycling. One user on a support forum said FES cycling kept his leg muscles from wasting away after his T6 injury. But he also said the $5,000 price tag for a home unit was too high. Then there are exoskeletons. Devices like Ekso and ReWalk let people with complete paraplegia stand and take steps. One Reddit user got his first steps in three years using one. But those sessions are limited to 25-45 minutes. They’re exhausting. And they need two or three therapists to help you stay safe. For upper limbs, robotic arms like Armeo help people with cervical injuries practice reaching, grasping, and releasing. These aren’t toys. They’re precision tools that track your movement and adjust resistance in real time. And then there’s the new frontier: implantable devices. In 2022, the FDA approved a diaphragm pacing system that helps people with high cervical injuries breathe without a ventilator. It cuts ventilator dependence by 74%. Brain-computer interfaces are in early trials-some patients have regained 38% hand function just by thinking about moving.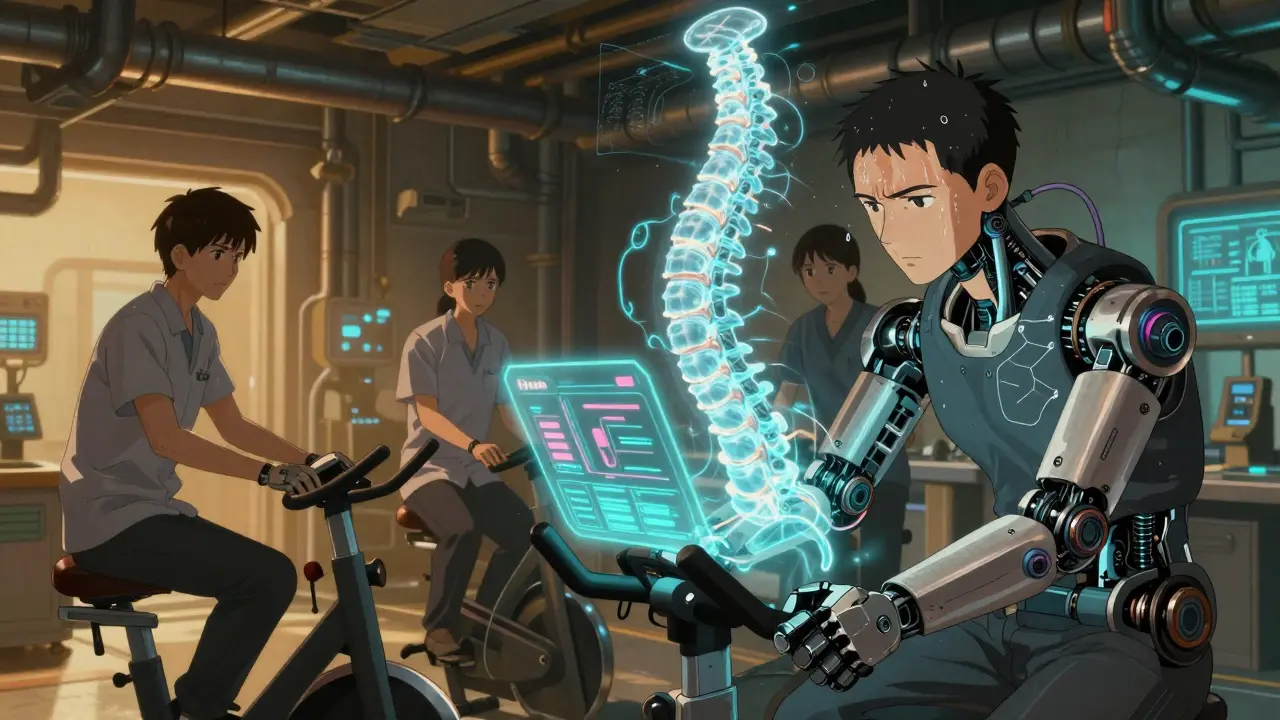
What Works Best? The Evidence
Not all rehab is created equal. Treadmill training with body weight support has been shown to improve walking speed 23% more than regular walking practice for incomplete injuries. Why? Because it trains your brain’s walking circuits in a way that mimics natural movement. Spasticity-those sudden, painful muscle spasms-is a huge problem. Up to 78% of people with SCI deal with it. The best approach? Combine medicine like baclofen with targeted Botox injections. Mayo Clinic reports this combo reduces spasticity scores by 40-60% in nearly 8 out of 10 patients. But here’s the catch: many of these high-tech tools are expensive. Medicare covers 80% of standard wheelchairs after your deductible, but specialized seating systems can cost $1,200 to $3,500 out of pocket. Most insurance plans won’t cover home FES bikes or exoskeletons. And even when they do, you’re lucky if you get 10 sessions a year.The Real Challenges: Bladder, Bowel, and Burnout
The hardest parts of recovery aren’t the flashy machines. They’re the daily grind. Neurogenic bladder and bowel take 45 to 90 minutes every day to manage. Catheterization. Suppositories. Digital stimulation. It’s messy. It’s tiring. And if you don’t do it right, you risk kidney damage or life-threatening infections. Caregivers get worn down too. Improper transfers cause 32% of shoulder injuries in family members or nurses who help lift and move you. That’s why training isn’t just for the patient-it’s for everyone around you. And then there’s motivation. A survey found 68% of people quit their home exercise programs within six months. Why? No one’s checking in. No one’s pushing them. No one’s celebrating small wins. Peer support changes that. At Spaulding Rehabilitation, 82% of patients said talking to someone who’d been through the same thing made them feel less alone. That’s not therapy. That’s human connection.
Where the Field Is Headed
The SCI rehab market is growing fast-projected to hit $2.6 billion by 2028. More centers are using AI to personalize therapy plans. Telehealth follow-ups are now standard at 73% of top programs. That’s huge for people who live far from specialized hospitals. But funding is still a wall. Medicare pays only 83% of what it actually costs to run a rehab program. That means hospitals lose money on every patient. And because only 32% of general hospitals offer full SCI programs, many people end up in places that don’t have the right tools, the right staff, or the right experience. The future isn’t just about better machines. It’s about better access. Better training for caregivers. Better mental health support. And better insurance policies that don’t treat recovery as a luxury.What You Can Do Right Now
If you or someone you love has a spinal cord injury:- Start rehab as soon as you’re medically stable-don’t wait.
- Ask about FES, exoskeletons, and robotic therapy. Even if insurance won’t cover it, some centers offer trial sessions.
- Find a peer mentor. The Christopher & Dana Reeve Foundation has a free network of people who’ve lived through it.
- Learn proper transfer techniques. Ask for a caregiver training session-it could prevent a lifelong injury.
- Track your bowel and bladder routine. Write it down. Set alarms. This isn’t optional.
- Push for home modifications. Ramps, grab bars, roll-in showers-these aren’t nice-to-haves. They’re necessities.
Can you walk again after a spinal cord injury?
It depends on the injury. For complete injuries, only 1-3% of people with paraplegia regain the ability to walk. For incomplete injuries, up to 59% can regain walking function with intensive rehab. Technologies like exoskeletons and FES-assisted treadmill training help many people stand and take steps, even if they can’t walk independently long-term. The key is early, consistent therapy.
How long does spinal cord injury rehab last?
Rehab is lifelong, but the most intense phase lasts 6 to 12 weeks in an inpatient setting. After that, most people move to outpatient care, with 2-3 therapy sessions per week. Even years later, people continue daily exercises, adaptive training, and health management. The first year is critical for maximizing recovery, but improvements can continue for years with consistent effort.
What’s the difference between complete and incomplete spinal cord injuries?
A complete injury means no sensory or motor function remains below the injury level. An incomplete injury means some signals still pass through the damaged area. People with incomplete injuries have a much higher chance of regaining movement, sensation, or function. Recovery potential is significantly greater with incomplete injuries-up to 80-90% of functional ability can return in the first year with proper rehab.
Are exoskeletons worth the cost?
Exoskeletons like Ekso and ReWalk are expensive-often over $100,000-and insurance rarely covers them for home use. But in a rehab center, they can be life-changing. They help rebuild muscle memory, improve circulation, reduce spasticity, and boost mental health by giving users the experience of standing and walking again. For many, the emotional benefit outweighs the cost. However, they’re not a cure. They’re a tool-and only effective with trained therapists and consistent use.
How do you manage bladder and bowel issues after SCI?
Bladder management usually involves scheduled catheterization every 4-6 hours. Bowel programs include digital stimulation, suppositories, or enemas, often done at the same time daily to train the body. It takes 45-90 minutes each day and must be consistent to avoid infections or blockages. Many people use apps or alarms to stay on schedule. A urologist or continence nurse can help design a personalized plan.
Can you prevent complications like pressure sores?
Yes, but it takes daily effort. You must shift your weight every 15-30 minutes when sitting. Use a pressure-relieving cushion. Check your skin every day for redness or sores-especially on tailbone, hips, heels, and shoulder blades. Keep skin clean and dry. If you notice a sore that doesn’t fade after 15 minutes of pressure relief, see a doctor immediately. Pressure sores can become life-threatening if they reach bone.
What role does mental health play in SCI recovery?
Mental health is just as important as physical rehab. Depression, anxiety, and grief are common after SCI. Studies show that patients who get peer counseling are 82% more likely to adjust well to life after injury. Therapy, support groups, and staying connected to community are essential. Recovery isn’t just about mobility-it’s about rebuilding identity, purpose, and hope.
Is there a cure for spinal cord injury?
There is no cure yet. But the field is advancing fast. Implantable diaphragm pacers, brain-computer interfaces, and nerve regeneration therapies are showing real promise in clinical trials. The focus now is on maximizing function through rehab and technology. While a full cure may still be years away, many people today live fuller, more independent lives than ever before thanks to modern interventions.


Lance Nickie
January 14, 2026 AT 01:16spinal cord what? i just want my phone to charge faster lol
Gregory Parschauer
January 14, 2026 AT 15:27Let me be perfectly clear: the systemic neglect of spinal cord injury rehabilitation in this country is a moral catastrophe wrapped in bureaucratic indifference. We’re deploying $100K exoskeletons while patients are left to catheterize on linoleum floors in underfunded county hospitals. The FDA approves diaphragm pacers but denies coverage for home FES bikes because they’re ‘non-essential’? That’s not healthcare-that’s eugenics by insurance formulary. The real tragedy isn’t the injury-it’s the society that treats recovery as a privilege for those who can afford it, not a human right. And don’t even get me started on how caregiver burnout is normalized as ‘part of the journey.’ It’s not a journey. It’s a death sentence for families without resources.
Someone needs to sue the AMA. Someone needs to burn down the CMS policy manual. And until that happens, we’re not rehabilitating patients-we’re just managing their slow, quiet decay.
And yes, I’ve seen it firsthand. My brother was T4. He died at 32 from a pressure ulcer that went untreated for 14 days because Medicaid wouldn’t approve a specialty cushion. Don’t talk to me about ‘hope’ or ‘resilience.’ Talk to me about funding.
Until then, I’m not ‘inspired.’ I’m furious.
And if you’re reading this and you’re not screaming about this too, you’re part of the problem.
Stop scrolling. Start protesting.
James Castner
January 16, 2026 AT 02:52While the clinical and technological advancements outlined here are indeed profound and warrant serious academic consideration, I find myself compelled to interrogate the underlying epistemological framework that governs our current paradigm of spinal cord injury rehabilitation. The very notion of ‘recovery’ as a linear, quantifiable trajectory toward a pre-injury state is, in my view, a deeply anthropocentric fallacy-one that privileges neurotypical mobility as the sole metric of human value. What if, instead of attempting to ‘restore’ function, we were to radically reimagine embodiment itself? The exoskeleton, for instance, is not merely a prosthetic device; it is a phenomenological extension of the will, a cyborgian reconfiguration of agency that challenges the Cartesian dichotomy between body and mind. When a patient stands through mechanical augmentation, they are not merely walking-they are performing a radical act of ontological reclamation.
Moreover, the commodification of rehabilitation technologies under capitalist healthcare structures reveals a deeper pathology: the reduction of human dignity to actuarial risk models. The fact that a $5,000 FES bike is deemed ‘non-essential’ while pharmaceuticals for erectile dysfunction receive blanket coverage is not an oversight-it is a moral indictment. We must shift from a model of ‘functional restoration’ to one of ‘existential flourishing.’ This requires not just policy reform, but a cultural revolution in how we perceive disability-not as deficit, but as divergence.
And yet, I remain cautiously optimistic. The emergence of brain-computer interfaces, though nascent, suggests that the boundary between neural intention and external action may soon dissolve entirely. Perhaps the future of SCI rehabilitation lies not in repairing the spinal cord, but in transcending it.
Adam Rivera
January 16, 2026 AT 22:26Hey, just wanted to say this post hit different. I’m from rural Kentucky and my cousin had a T6 injury last year. We didn’t even know where to start-no one in our town had heard of FES or exoskeletons. We found a nonprofit that hooked him up with a trial at a rehab center 3 hours away, and honestly? The first time he stood up with that ReWalk, he started crying. Not because he could walk, but because he felt like himself again for five minutes.
My aunt still has to do his catheter schedule on a sticky note because he forgets. And yeah, insurance won’t cover the fancy wheelchair cushion. But we got a used one off Facebook Marketplace for $150. It’s not perfect, but it’s better than nothing.
Don’t underestimate the power of a friend showing up with coffee and a new set of catheters. That’s the real rehab right there.
Also, if anyone’s in the South and needs help navigating insurance, DM me. I’ve become a reluctant expert.
Rosalee Vanness
January 17, 2026 AT 18:08There’s something so quietly heroic about the daily rituals no one talks about-the alarm at 6 a.m. for bowel care, the way your fingers learn the exact angle to tilt the catheter so it doesn’t sting, the silent battle of relearning how to hug without crushing someone’s ribs, the way you start noticing the texture of your own skin like it’s a foreign landscape you’re learning to map.
I’ve been living with an incomplete T10 injury for eight years now. The first year was all about rage and grief. The second year was about learning to ask for help without feeling like a burden. The third year? I started teaching myself to use my residual hand function to hold a paintbrush. Now I make abstract pieces with my feet and wrists. One sold last month. I didn’t tell anyone I painted it. I just signed it ‘T10’.
People think rehab is about walking again. But for so many of us, it’s about learning how to live inside a body that doesn’t obey you anymore-and still choosing to create, to laugh, to love, to be stubbornly, beautifully alive. You don’t need a $100K exoskeleton to do that. You just need to stop waiting for permission to be whole.
And if you’re a caregiver? You’re not just helping someone. You’re holding space for someone’s soul to keep breathing. That’s sacred work. Don’t let anyone tell you otherwise.
lucy cooke
January 18, 2026 AT 05:35Oh, darling, how quaint. You speak of ‘rehabilitation’ as if it were some noble pilgrimage when in truth, it’s merely the grotesque theater of late-stage capitalism’s last gasp. We have turned human suffering into a boutique experience-FES bikes for the affluent, catheter schedules for the proletariat. How poetic that the very machines meant to restore autonomy are priced beyond the reach of those who need them most. The exoskeleton? A gilded cage for the middle class. The diaphragm pacer? A luxury accessory for the spinal elite.
And let us not forget the performative empathy of ‘peer mentors’-how convenient that we’ve outsourced emotional labor to the traumatized themselves. ‘Talk to someone who’s been through it!’ as if trauma were a club you could join and then monetize with a nonprofit grant.
Meanwhile, the real revolution is happening in the quiet corners: the woman in Ohio who mods a wheelchair with a bicycle chain to self-propel; the veteran in Texas who uses a Wii remote to control a robotic arm. No FDA approval. No insurance. Just ingenuity forged in desperation.
Rehab isn’t about technology. It’s about rebellion.
And we, the broken, are the most revolutionary of all.
Trevor Davis
January 18, 2026 AT 21:37I just want to say-this is the most comprehensive, respectful, and beautifully written piece on SCI I’ve ever read. I’m a nurse in a rehab unit, and I’ve seen everything from full recovery to heartbreaking decline. What you’ve captured here isn’t just medical info-it’s truth. The bladder routines, the caregiver strain, the silent grief. I’ve held patients while they cried because they couldn’t feel their own foot. I’ve watched spouses break down because they didn’t know how to lift them anymore.
I also want to add: if you’re reading this and you’re scared, it’s okay. I’ve had patients who thought they’d never laugh again. Now they’re doing TikTok dances from their wheelchairs. One guy started a podcast called ‘Spinal Cord & Sass.’
You’re not broken. You’re adapting. And that’s the bravest thing a human can do.
Thank you for writing this. It’s helping people like me feel less alone too.
John Tran
January 20, 2026 AT 05:38Okay so i was at a rehab center last year and the guy next to me had a C5 injury and he was like ‘i just wanna feel my toes again’ and i was like bro that’s so deep and then i found out he was on a fes bike and he could pedal for 20 mins and he cried because he felt his legs tingle for the first time in 4 years and i thought wow this tech is wild but then i looked at the bill and it was 50k and i was like wait this is insane how is this not covered like why is a machine that lets someone feel their body not a basic human right like wtf is wrong with america
also i saw a girl do her own catheterization and she was like ‘i do it while watching cat videos’ and i was like that’s the most human thing i’ve ever seen and i started crying in the hallway and no one noticed
we’re all just trying to not die while learning how to live again
ps i think the exoskeleton is kinda hot tbh
mike swinchoski
January 21, 2026 AT 11:42You people act like this is some miracle. My cousin got hurt and now he can't even wipe his own butt. You think a $100K robot fixes that? Nah. He needs someone to help him go to the bathroom every day. That's the real issue. No one talks about that. Just fancy machines and feel-good stories. The truth? Most people end up in nursing homes. Get real.