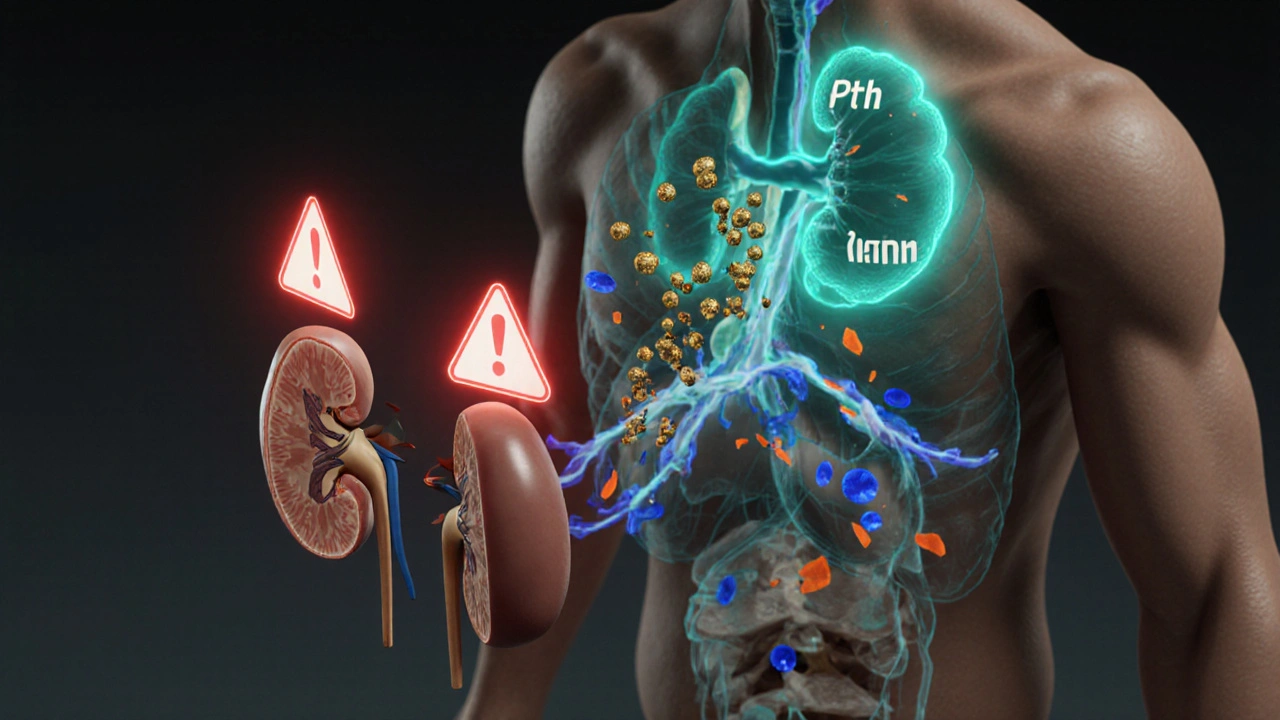
Secondary Hyperparathyroidism Explained
When dealing with Secondary Hyperparathyroidism, a condition where the parathyroid glands overproduce hormone in response to low calcium or vitamin D levels. Also known as renal secondary hyperparathyroidism, it most often shows up in people with Chronic Kidney Disease, a long‑term loss of kidney function that disrupts mineral balance. The kidneys can’t convert enough vitamin D to its active form, leading to Vitamin D Deficiency, low levels of the hormone that helps absorb calcium from food. In response, the parathyroid glands crank up production of Parathyroid Hormone, the regulator that raises blood calcium by pulling it from bones and kidneys. This chain reaction creates the classic triad of high PTH, low calcium, and high phosphate that doctors watch for in labs. Understanding how these pieces fit together helps you see why managing kidney health, vitamin D, and phosphate intake is the first line of defense against the condition.
How to Treat and Control the Condition
Modern therapy targets the root causes rather than just the symptoms. secondary hyperparathyroidism can be tamed with Calcimimetics, drugs that trick the parathyroid glands into thinking calcium levels are higher than they really are, which lowers PTH output without raising calcium too much. Phosphate Binders, medications that attach to dietary phosphate in the gut and prevent its absorption, are another cornerstone, especially for patients on dialysis. Active vitamin D analogs, such as calcitriol, supplement the missing hormone and help keep calcium moving into the blood where it belongs. Together, these treatments can improve Bone Mineral Density, a measure of bone strength that often drops when PTH stays high for long periods, and reduce the risk of cardiovascular calcification that plagues many kidney patients. Lifestyle tweaks—cutting down on processed foods high in phosphate, staying active, and monitoring fluid intake—amplify the drug effects and keep the whole system more stable.
Regular monitoring ties everything together. Doctors track Serum Calcium, the amount of calcium circulating in the blood, and Serum Phosphate, the level of phosphorus in the bloodstream, alongside PTH levels to gauge how well the therapy is working. Adjustments to calcimimetics or phosphate binders happen quickly if labs drift out of range. Nutrition counseling focuses on low‑phosphate foods like fresh fruits, vegetables, and unprocessed meats while encouraging adequate protein to maintain muscle mass. With a solid plan that blends medication, diet, and routine lab checks, patients can keep secondary hyperparathyroidism in check and avoid the bone and heart complications that often follow. Below you’ll find a curated set of articles that dive deeper into each of these topics, from the science behind calcimimetics to practical tips for low‑phosphate cooking.
- October
17
2025 - 5
Secondary Hyperparathyroidism and GI Problems: What’s the Link?
Explore how secondary hyperparathyroidism triggers nausea, constipation, and other gut problems, and learn practical steps to manage both the hormonal disorder and digestive health.
Read More