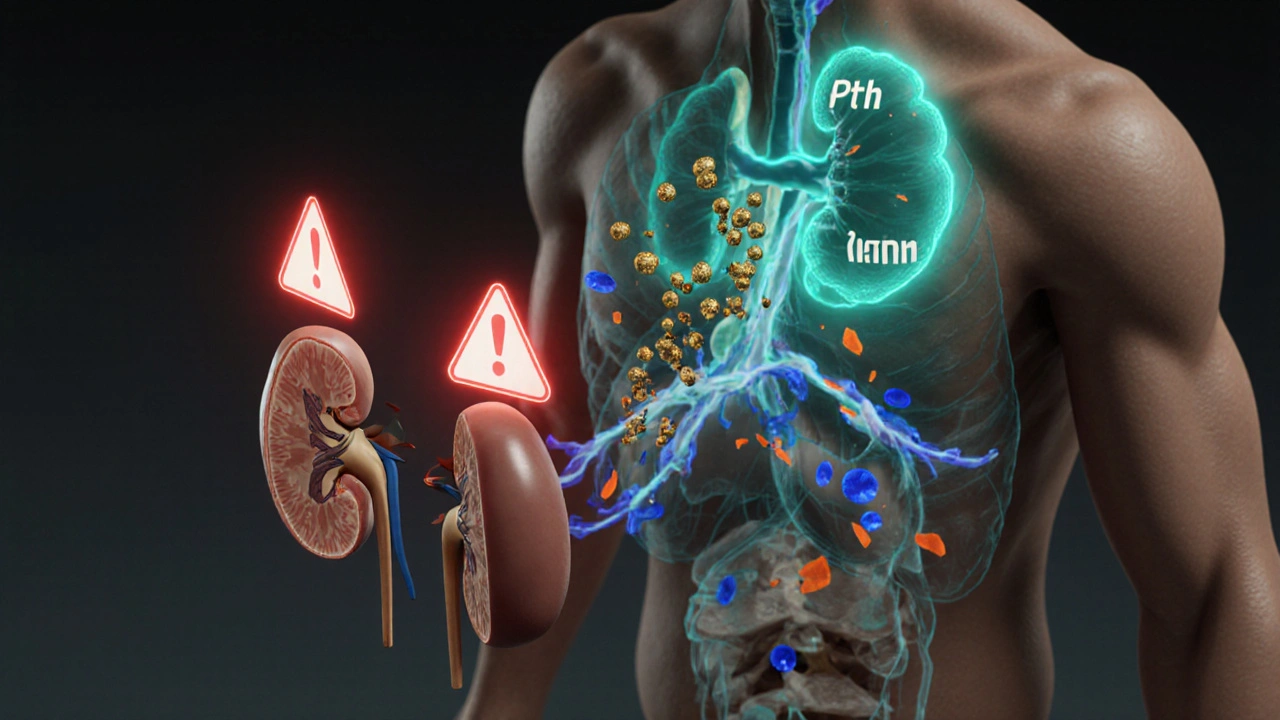
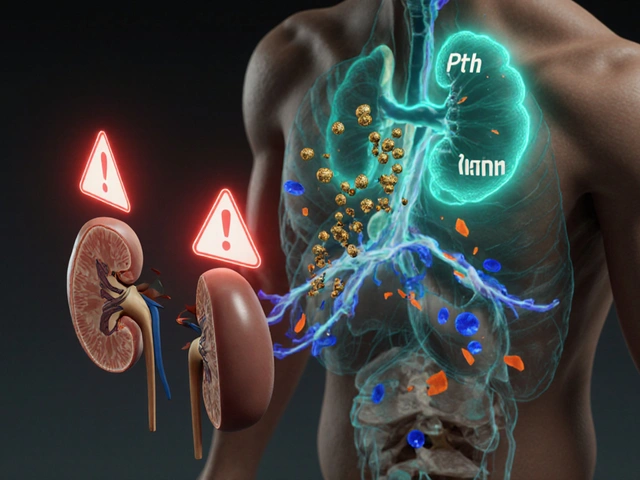
Phosphate Binder Selector for Secondary Hyperparathyroidism
Ever wondered why patients diagnosed with secondary hyperparathyroidism often complain about stomach upset, nausea or constipation? The connection isn’t a coincidence - the hormonal imbalance that drives bone disease can also tip the gut’s delicate chemistry. Below we unpack the biology, pinpoint the most common digestive complaints, and give you practical steps to keep the gut happy while managing the endocrine disorder.
What Is Secondary Hyperparathyroidism?
Secondary hyperparathyroidism is a condition in which the parathyroid glands release excessive parathyroid hormone (PTH) in response to low calcium, high phosphate, or low vitamin D levels. It’s most frequently seen in people with chronic kidney disease (CKD), where the kidneys can’t activate vitaminD or excrete phosphate efficiently.
What Counts as Gastrointestinal Issues?
Gastrointestinal issues cover any disorder that affects the stomach, intestines, or related organs - from occasional heartburn to chronic constipation, abdominal pain, nausea, vomiting, and malabsorption.
Why the Tie‑In? The Core Physiology
Understanding the link starts with parathyroid hormone. PTH raises blood calcium by pulling calcium from bone, telling kidneys to retain calcium, and prompting the activation of vitaminD, which in turn boosts intestinal calcium absorption. At the same time, PTH pushes the kidneys to dump phosphate. When the kidneys falter (as in CKD), phosphate builds up, triggering even more PTH release.
Two downstream pathways touch the gut directly:
- Calcium metabolism: Elevated calcium in the intestinal lumen can stiffen smooth muscle, leading to constipation. Conversely, low calcium can increase gut motility, causing diarrhea.
- Phosphate binders: To control hyperphosphatemia, many patients swallow calcium‑based binders (e.g., calcium carbonate). These tablets act like antacids, neutralizing stomach acid and often slowing gastric emptying, which shows up as bloating, nausea, and constipation.
Common GI Symptoms in Secondary Hyperparathyroidism
Clinical observations repeatedly flag a handful of gastrointestinal red flags in this population:
- Nausea and vomiting - especially after high‑dose vitaminD supplementation.
- Constipation - linked to calcium‑rich binders and mild hypercalcemia.
- Diarrhea - can stem from phosphate‑binding resins that alter the gut’s osmotic balance.
- Abdominal pain - a nonspecific but frequent complaint, often related to gastric distension from antacid‑type binders.
- Loss of appetite - secondary to nausea or early satiety caused by slowed gastric emptying.

Mechanistic Deep‑Dive
Let’s look at the main culprits, one by one.
1. Calcium Overload from Binders
Calcium‑based phosphate binders act as a double‑edged sword. While they lower serum phosphate, they also flood the intestine with calcium. In the small intestine, excess calcium can form insoluble soaps with fatty acids, leading to malabsorption of fat‑soluble vitamins and a greasy, loose stool picture. In the colon, the same excess calcium binds water, making stools hard and difficult to pass.
2. VitaminD Therapy
High‑dose cholecalciferol or calcitriol is a staple for CKD patients, but a rapid rise in active vitaminD spikes calcium absorption. When blood calcium climbs above the normal range, patients may develop hypercalcemia, which classic textbooks list as a cause of nausea, vomiting, and constipation.
3. Altered Intestinal Motility
PTH itself has a subtle effect on smooth‑muscle tone. Studies in animal models show that prolonged high PTH levels can desensitize the enteric nervous system, leading to irregular peristalsis. This helps explain why some patients present with mixed constipation‑diarrhea patterns.
4. Chronic Kidney Disease‑Related Metabolism
CKD reduces the clearance of many metabolites that act as gut irritants. Uremic toxins can increase gut permeability, allowing bacterial endotoxins to trigger low‑grade inflammation. The result is a background of abdominal discomfort that may be mistakenly blamed on the endocrine disorder.
Practical Checklist for Clinicians
When you see a CKD patient with secondary hyperparathyroidism, run through this quick list to catch GI issues early:
- Check serum calcium, phosphate, and PTH levels - look for trends, not just static values.
- Ask about bowel habits: frequency, consistency, presence of blood or mucus.
- Review phosphate‑binder type and dose - consider switching to non‑calcium binders (e.g., sevelamer) if constipation is prominent.
- Assess vitaminD dosage - titrate down if hypercalcemia develops.
- Screen for uremic symptoms that may mimic gastrointestinal disease (e.g., nausea from metabolic acidosis).
- Consider a trial of a calcimimetic (e.g., cinacalcet) to lower PTH without increasing calcium load.
Comparison Table: GI Symptoms in Secondary Hyperparathyroidism vs. Other Common Causes
| Condition | Primary Driver of Symptoms | Typical Constipation/Diarrhea Pattern | Key Labs |
|---|---|---|---|
| Secondary Hyperparathyroidism | Calcium‑based binders + PTH‑mediated motility changes | Mixed - often constipation; occasional diarrhea from binders | ↑PTH, ↑Phosphate, variable Ca |
| Iron‑deficiency anemia | Reduced mucosal oxygenation | Often constipation | ↓Hb, ↓Ferritin |
| Irritable Bowel Syndrome | Visceral hypersensitivity | Either predominant constipation or diarrhea | Normal labs |
| Hypercalcemia (primary) | Excess serum calcium | Constipation predominate | ↑Serum Ca, ↓PTH |
Managing the Gut While Treating the Gland
Therapeutic goals for secondary hyperparathyroidism are clear: keep PTH, calcium, and phosphate within target ranges. But you can also protect the gut:
- Choose the right binder: For patients plagued by constipation, switch to sevelamer or lanthanum carbonate, which don’t add calcium.
- Hydration and fiber: Encourage at least 2L of fluid daily and 25‑30g of dietary fiber to offset the constipating effect of calcium.
- Calcium‑sparing vitaminD regimens: Use modest doses of active vitaminD and monitor serum calcium weekly during titration.
- Calcimimetics: Agents like cinacalcet lower PTH without raising calcium, often reducing the need for high‑dose binders.
- Probiotic support: Some small trials suggest that lactobacillus‑based probiotics improve bowel regularity in CKD patients on binders.
When to Refer to a Gastroenterologist
If any of the following appear, bring a gut specialist into the loop:
- Persistent constipation despite fiber and binder change (more than 4weeks).
- Unexplained weight loss or occult GI bleeding.
- Severe abdominal pain with guarding - could signal bowel obstruction from hardened calcium carbonate tablets.
- Recurrent episodes of diarrhea that impair electrolyte balance.
Bottom Line
The gut and the parathyroid gland talk to each other through calcium, phosphate, and the medications we use to keep those minerals in check. By recognizing the patterns - nausea after vitaminD spikes, constipation from calcium binders, or mixed bowel habits from PTH‑driven motility changes - you can treat secondary hyperparathyroidism without sending the digestive system into chaos.
Frequently Asked Questions
Why do calcium‑based phosphate binders cause constipation?
These binders add extra calcium to the intestinal lumen. Calcium binds water and forms hard stools, especially when the patient’s diet is low in fiber. Switching to a non‑calcium binder usually resolves the problem.
Can vitaminD therapy make nausea worse?
Yes. High doses of active vitaminD increase calcium absorption, which can push serum calcium into the upper‑normal range. Hypercalcemia irritates the stomach lining, leading to nausea, vomiting, and loss of appetite.
Is it safe to stop phosphate binders if I have constipation?
Abruptly stopping binders raises serum phosphate, which in turn worsens secondary hyperparathyroidism. The better approach is to switch to a non‑calcium binder or reduce the calcium dose while adding fiber and fluids.
How does PTH affect intestinal motility?
Prolonged high PTH levels can dampen the responsiveness of the enteric nervous system, leading to irregular peristalsis. Clinically this shows up as alternating constipation and diarrhea, especially when other triggers like binders are present.
When should I consider a calcimimetic?
If PTH remains elevated despite optimal phosphate control, or if calcium‑based binders are causing intolerable GI side‑effects, a calcimimetic such as cinacalcet can lower PTH without adding calcium load.
Mary Davies
October 17, 2025 AT 02:16I keep circling the idea that calcium binders act like tiny anchors in the gut, pulling the rhythm of digestion into a slow, stubborn crawl. The drama of excess calcium turning smooth muscle into stone‑like tension is almost theatrical, and patients feel it in every sluggish bowel movement. It’s a reminder that fixing the bones can unintentionally tie knots in the intestines.
Emily (Emma) Majerus
October 20, 2025 AT 13:36Great rundown! Just tweak the binder dose if your stool gets hard, definatly keep an eye on fiber.
Virginia Dominguez Gonzales
October 24, 2025 AT 00:56This is a solid guide, and I love how you frame the gut‑parathyroid connection as a story of balance. When we step in with supportive coaching, we can help patients navigate the calcium cliffs and phosphate valleys. A little extra water, a dash of fiber, and the right binder can turn chaos into calm.
Kevin Adams
October 27, 2025 AT 11:16The gut whispers to the glands, a silent pact of minerals and motion; we ignore it at our peril.
Sara Werb
October 30, 2025 AT 22:36Listen up!!! The pharma elite don’t want you to know that calcium binders are basically tiny time‑bombs for your gut!!! They hide the side‑effects behind glossy pamphlets while the real agenda is to keep you hooked on endless prescriptions!!! Every time you swallow a carbonate tablet you’re signing a contract with the big brother of the medical industry!!! They claim it’s for phosphate control, but the truth is buried in hidden data!!! Don’t be a pawn, read the fine print and demand alternatives!!!
Winston Bar
November 3, 2025 AT 09:56Honestly, this whole thing sounds overhyped. Most patients just have a bit of belly pain; no need for all this fancy talk. I think the meds are fine as they are.
Russell Abelido
November 6, 2025 AT 21:16I hear you, and it’s heartbreaking how a treatment meant to protect bones can clog the gut’s harmony. Think of the intestine as a river, and calcium as rocks that change its flow. 🌊 When the rocks multiply, the water slows, and the whole ecosystem feels the strain. Let’s keep listening to those subtle cues and adjust the meds with care.
Emily Rankin
November 10, 2025 AT 08:36The dance between parathyroid hormone and our digestive tract is a reminder that the body seeks equilibrium. Every adjustment we make is a step toward that perfect balance, and with mindful choices we can usher in comfort and health.
genevieve gaudet
November 13, 2025 AT 19:56From a holistic view, many traditional diets naturally modulate calcium and phosphate without heavy binders. Think about how Mediterranean meals blend leafy greens, legumes, and modest dairy – a gentle way to keep the gut and glands in sync. It’s worth exploring those culinary wisdoms alongside modern therapy.
Patricia Echegaray
November 17, 2025 AT 07:16Picture this: a secret cabal of nutrient‑gatekeepers manipulating the very chemistry of our bloodstreams! They sprinkle calcium in our meds like glitter, hoping we’ll be too distracted by the sparkle to notice the sluggishness creeping through our bowels. It’s a vivid tableau of control, and only the vigilant can break free.
Miriam Rahel
November 20, 2025 AT 18:36In accordance with the prevailing nephrological literature, hyperphosphatemia management necessitates a nuanced appraisal of binder selection, dosage, and patient-specific gastrointestinal tolerance. Empirical data substantiate that non‑calcium phosphate binders mitigate constipation prevalence, thereby optimizing therapeutic outcomes.
Samantha Oldrid
November 24, 2025 AT 05:56Oh sure, because ignoring constipation totally solves the calcium problem 🙄.
Malia Rivera
November 27, 2025 AT 17:16While the gut may whisper, it also shouts the truth about our body's allegiance to a balanced diet-something our ancestors prized. If we continue to flood ourselves with synthetic binders, we betray that heritage. A more patriotic approach would be to prioritize natural sources and minimal intervention.
lisa howard
December 1, 2025 AT 04:36When Winston declares that the concerns are overblown, I feel like a chorus of silent sufferers is being dismissed in the shadows of complacency. The reality is that each tablet of calcium carbonate is a miniature brick, building a fortress of constipation that traps the vitality of the patient. Imagine a river clogged with stones; the water still moves, but with effort, and eventually it may overflow or dry up. Those who ignore the subtle signs-bloating, nausea, a slow march to the bathroom-are amplifying the very problem they claim is negligible. Moreover, the psychological toll of chronic discomfort cannot be reduced to a mere inconvenience; it seeps into daily life, affecting mood, work, and relationships. The medical community, in its haste to control phosphate, may inadvertently craft a new epidemic of gastrointestinal distress. Studies have shown that patients on high‑dose calcium binders report higher rates of constipation and abdominal pain, a fact often buried beneath promotional literature. We must ask ourselves whether the trade‑off truly serves the patient’s holistic well‑being. A balanced protocol that incorporates non‑calcium binders, dietary fiber, and patient education could dissolve the barricade that has formed. It is not an attack on renal therapy, but an evolution toward patient‑centered care. Each physician has the power to rewrite the narrative, replacing the status quo of “just take your pills” with a symphony of attentive management. Let us not be content with the status quo when innovation beckons. By listening to the gut’s cries, we honor the very organ that sustains us. The path forward demands humility, curiosity, and a willingness to adjust our prescriptions for the greater good. Together, we can turn the tide and restore harmony between bone and bowel.
Cindy Thomas
December 4, 2025 AT 15:56While Samantha’s sarcasm hints at a deeper truth, the data actually show that constipation rates jump noticeably with calcium carbonate-something we can't just brush off. It’s essential to weigh the evidence rather than rely on witty quips. 😊
Carissa Padilha
December 8, 2025 AT 03:16The alarmist tone of Sara’s post might feel like a tinfoil hat, but there’s a grain of reality in the claim that binders can overwhelm the gut. Some manufacturers have indeed downplayed gastrointestinal side‑effects to keep sales high. Yet, not every binder is a villain; sevelamer, for example, sidesteps calcium‑related constipation. Still, we must stay vigilant and demand transparent reporting. The truth likely sits somewhere between sensationalism and omission.
Darryl Gates
December 11, 2025 AT 14:36Great point about traditional diets, Darryl-incorporating those food patterns can indeed help modulate mineral intake while supporting gut health.