Ever looked at your prescription bottle and felt confused by the little symbols and colored stickers? You’re not alone. Those tiny icons on your medicine label aren’t just decoration-they’re life-saving alerts designed to stop you from making dangerous mistakes. But here’s the problem: pharmacy warning icons often don’t work the way they’re supposed to. Many people misread them. Some ignore them. Others think they understand them-until they don’t.
What Are Pharmacy Warning Icons and Why Do They Exist?
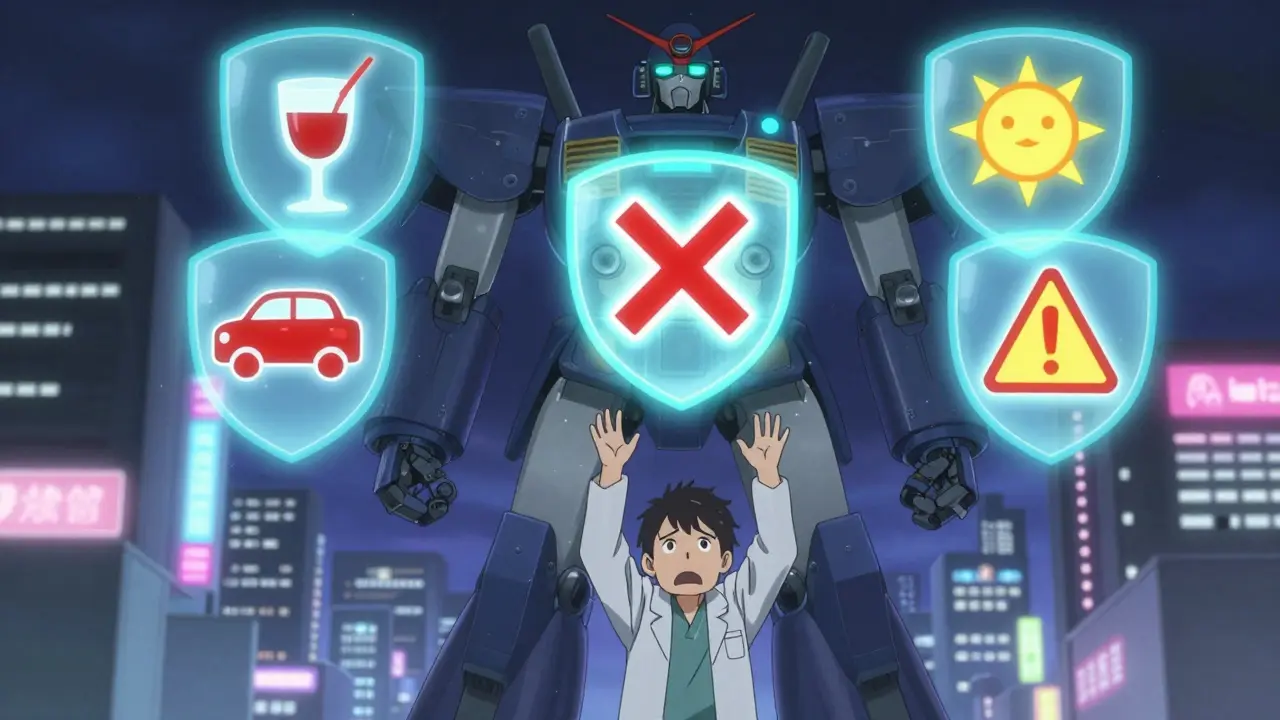
Pharmacy warning icons are visual cues placed on medication containers to quickly communicate safety risks. They’re meant to be understood at a glance, even if you can’t read well, don’t speak English, or are tired, stressed, or in pain. These icons include symbols like a drinking glass with a slash through it (meaning “avoid alcohol”), a car with a stop sign (meaning “don’t drive”), or a sun with a warning triangle (meaning “may cause sun sensitivity”). They were developed over decades by groups like the Institute for Safe Medication Practices (ISMP) and the U.S. Food and Drug Administration (FDA) to cut down on medication errors. In the U.S. alone, these errors lead to at least 7,000 deaths every year. That’s why pharmacies started using standardized labels in the mid-2000s. Today, about 90% of prescription bottles in the U.S. carry at least one warning icon. But standardization isn’t perfect. In the U.K., there are just nine official warning symbols used nationwide. In New Zealand, they use a simple yellow sticker system with clear text. In the U.S.? It’s a mess. CVS uses 14 different icons. Walgreens uses 17. Independent pharmacies? Some use over 20. That inconsistency makes it harder for patients to learn what anything means.What the Colors Mean (and Why They Can Trick You)
Color plays a big role in how people interpret these warnings. Most patients assume red means “danger,” yellow means “caution,” and white or green means “just a suggestion.” That’s not always true. In many U.S. pharmacies, yellow stickers are used for drugs that make you sleepy-like beta blockers or sleep aids. But in some places, yellow is used for antibiotics. Tan stickers are supposed to mean “anti-infective,” but patients rarely notice the difference. A 2019 study found that 42% of people judge how serious a warning is based on color alone. That’s dangerous. A red label might say “take with food,” while a yellow one might say “can cause fatal liver damage.” The color doesn’t match the risk. Even worse, some symbols are completely misunderstood. One common icon-a circle with a line through it and a dropper inside-is meant to say “for external use only.” But 68% of patients with low health literacy thought it meant “do not use.” One Reddit user shared that their mother took eye drops by mouth because she thought the dropper symbol meant it was meant to be swallowed. That’s not a rare mistake. It’s a pattern.The Most Common Warning Icons and What They Really Mean
Here’s what the most frequent icons actually mean-based on FDA and ISMP guidelines:- Drinking glass with a slash: Avoid alcohol. Mixing alcohol with certain medications can cause dizziness, liver damage, or even death.
- Car with a red X: Do not drive or operate heavy machinery. This applies to painkillers, sleep meds, anxiety drugs, and even some antihistamines.
- Sun with a warning triangle: May cause sun sensitivity. You can get a bad sunburn or rash even with minimal exposure.
- Hand with a clock: Take at the same time every day. Missing doses can make the drug less effective or cause withdrawal.
- Food plate with a plus sign: Take with food. This helps your body absorb the drug better and reduces stomach upset.
- Tablet with a line through it: Do not crush, chew, or break. Some pills are designed to release slowly. Crushing them can cause an overdose.
- Stethoscope with a red slash: May interact with other medications. This is often paired with a list of drugs to avoid.
Why Patients Still Get It Wrong
You’d think that after years of using these icons, people would get used to them. But research shows otherwise. A 2021 Consumer Reports survey found that over half of Americans misinterpret at least one common warning. Why? First, too many labels. Pharmacies often slap on every possible warning-just in case. One bottle might have seven different stickers. That’s clutter. When everything screams “warning,” nothing stands out. Patients start ignoring them all. Second, small print. The FDA says critical warnings must be at least 6-point font. But on a tiny bottle, 6-point is barely readable. Seniors with poor eyesight? They can’t see it. Third, cultural differences. Symbols that make sense in the U.S. might mean something else elsewhere. The “radioactive” symbol used for “external use only” is a perfect example. People think it means “dangerous radiation,” not “don’t swallow.” And then there’s the false sense of security. A 2020 study found that 41% of patients said they understood their labels-but when tested, they got the meaning wrong. They thought they knew what it meant. They didn’t.How Pharmacists Decide Which Warnings to Use
You might assume the pharmacist just picks a warning based on the drug. It’s not that simple. Pharmacists are trained to consider the patient. A 70-year-old with heart disease taking a blood pressure pill? They get the “avoid alcohol” and “don’t drive” warnings. A 25-year-old with no other health issues? Maybe just the “take with food” sticker. But studies show that 38.7% of pharmacists overuse warnings-applying every possible label just to be safe. That makes the important ones get lost. Large pharmacy chains now use computer systems that recommend only the top 1-3 most critical warnings per prescription. Independent pharmacies? Many still rely on memory or outdated charts. That’s why two people with the same drug might get completely different labels. Training matters too. New pharmacy techs need 8 to 12 weeks of supervised practice to get it right. But not all pharmacies invest in that. And in fast-paced settings, mistakes happen.What’s Changing-and What’s Coming
Good news: Change is coming. In September 2022, the FDA released draft rules proposing a national standard for 12 core warning icons. CVS and Walgreens have already pledged to reduce their systems to match by 2024. That’s a big step. Some pharmacies are testing new tech. Kaiser Permanente tried augmented reality labels: point your phone at the bottle, and a short video plays explaining the warning. In tests, patient understanding jumped from 58% to 89%. But here’s the catch: 24% of seniors don’t use smartphones regularly. So the physical label still has to work on its own. The University of Pittsburgh is testing AI-driven labels that customize warnings based on your age, health conditions, and even your phone’s camera settings (like brightness). If you’re nearsighted, the text gets bigger. If you’re on blood thinners, it adds a warning about NSAIDs. This isn’t science fiction-it’s already being piloted.What You Can Do Right Now
Don’t wait for the system to fix itself. Here’s how to protect yourself:- Ask. When you get your prescription, say: “What does this sticker mean?” Don’t assume.
- Read the text. Even if the symbol looks familiar, read the words. They’re legally required to be accurate.
- Take a photo. If the label is hard to read, snap a picture and zoom in later.
- Use free tools. The ISMP offers a free Medication Safety Self-Assessment tool online. The CDC’s “Every Dose Counts” campaign has printable guides.
- Don’t ignore the small print. If a warning says “Do not crush,” and your pill looks like it should be crushed? Call the pharmacy. Some pills are designed to be swallowed whole-crushing them can be deadly.
Final Thought: Icons Are Tools, Not Magic
Pharmacy warning icons were meant to be a safety net. But they’re only as strong as the person using them. They can’t replace a conversation with your pharmacist. They can’t fix bad design. They can’t fix clutter. The best warning system in the world won’t help if you don’t understand it. And if you don’t understand it, you’re not just risking your health-you’re risking your life.So next time you pick up your prescription, pause. Look at the icons. Read the words. Ask one question. That one moment could save you from a mistake no one else will catch.
What do the colors on pharmacy warning labels mean?
There’s no universal color code, but many patients assume red means danger, yellow means caution, and white or green means less important. In reality, color usage varies by pharmacy chain. Yellow is often used for sedating medications, but sometimes it’s used for antibiotics. Tan stickers are supposed to mean anti-infectives, but many patients don’t notice the difference. Colors are meant to catch your eye, not to tell you the exact risk. Always read the text next to the symbol.
Why do some pills have so many warning labels?
Pharmacists sometimes apply every possible warning to avoid liability, even if it’s not relevant to you. This creates clutter, which makes it harder to spot the most important warnings. Large pharmacy chains now use software to limit labels to 1-3 critical ones per prescription. Independent pharmacies may still use more. If you see too many, ask which ones are most important for your situation.
Can I ignore a warning if I’ve taken the medicine before without problems?
No. Warnings are based on the drug’s chemical properties, not your past experience. For example, if you’ve taken a painkiller before without drowsiness, that doesn’t mean it won’t happen now-especially if you’re older, taking other meds, or drinking alcohol. Your body changes. The drug’s interaction risk doesn’t.
What should I do if I don’t understand a warning icon?
Call your pharmacy or ask your pharmacist directly. Don’t guess. Many pharmacies offer free counseling sessions when you pick up new prescriptions. You can also use free resources like the ISMP’s Medication Safety Self-Assessment tool or the CDC’s “Every Dose Counts” guides. Understanding your meds isn’t optional-it’s essential.
Are warning icons the same in the UK and the US?
No. The UK uses a nationally standardized system with just nine warning icons, which reduced patient misinterpretation from 39% to 17% after implementation in 2015. The U.S. has no national standard-CVS uses 14 icons, Walgreens uses 17, and independent pharmacies often use over 20. This inconsistency makes it harder for people to learn what symbols mean, especially if they move between states or pharmacies.
Do warning icons help non-English speakers?
Yes, when designed well. The FDA found that pairing symbols with simple text reduces errors among non-English speakers by 40%. But symbols must be universally recognizable. For example, a dropper icon meaning “external use only” was misunderstood by 68% of patients with low health literacy. The best systems combine clear symbols with short, plain-language text in multiple languages.
Is it safe to crush a pill if it’s hard to swallow?
Never crush a pill unless the label or your pharmacist says it’s okay. Many pills are designed to release slowly over time. Crushing them can cause a dangerous overdose. Even if the pill looks like it should be crushed, it might be a time-release or enteric-coated tablet. If swallowing is hard, ask your doctor for a liquid form or a different pill.
Marilyn Ferrera
January 1, 2026 AT 08:51Icons aren't magic. They're a starting point. If you don't read the text? You're gambling with your life. And yes, I've seen people swallow eye drops because of that dropper symbol. It's not a joke. It's a systemic failure.
Robb Rice
January 2, 2026 AT 23:16I appreciate the thoroughness of this post, though I must note that the phrase 'don't crush' is often misinterpreted as 'don't take' by patients with limited literacy. A more standardized icon set would be ideal, though implementation remains inconsistent across providers.
Harriet Hollingsworth
January 4, 2026 AT 12:21People are lazy. They see a yellow sticker and think 'eh, it's not red, so it's fine.' Then they die. And we act shocked? No. This is on them. Stop blaming the system and start taking responsibility. Your life isn't a game show.
Deepika D
January 6, 2026 AT 00:17I come from a small town in India where pharmacists still hand-write instructions on slips of paper-and people understand them better than those with fancy icons here. Why? Because someone sat down, looked them in the eye, and said 'this is what you do.' No symbols. No clutter. Just human connection. We lost something when we outsourced care to stickers. I’ve taught my grandmother to read her pills by saying them out loud every morning. She never forgets. Maybe we need less tech and more touch.
Bennett Ryynanen
January 7, 2026 AT 17:58Bro, I had a friend almost OD because he crushed his extended-release oxycodone. The label said 'DO NOT CRUSH' in bold, but he thought it meant 'don't crush unless you're desperate.' He was DESPERATE. The icon? A tablet with a line through it. Looks like a 'no entry' sign. Of course he thought it was okay. This system is designed to fail. Stop pretending it's not broken.
Chandreson Chandreas
January 9, 2026 AT 05:45Honestly? I just point my phone at the bottle now. 😅 The AR thing at my pharmacy shows a 15-second video of a guy saying 'don't drink alcohol with this.' Way better than staring at a tiny sun with a triangle. My grandma still doesn’t get it, but she laughs when the video plays. Progress, not perfection. 🙌
Darren Pearson
January 9, 2026 AT 06:23The fundamental flaw lies in the epistemological assumption that visual semiotics can be universally decoded without linguistic scaffolding. The FDA’s draft standard, while a step forward, remains insufficiently grounded in cognitive psychology and cross-cultural semiotics. One must question whether iconography, divorced from context, can ever serve as a reliable heuristic for high-stakes medical communication.
Stewart Smith
January 10, 2026 AT 23:33So we’re spending millions on fancy symbols… and still, someone swallows eye drops? Wow. We really are brilliant at solving problems we created by overcomplicating everything. 🙃
Retha Dungga
January 12, 2026 AT 19:56The icons are just mirrors of our broken system we refuse to fix. We want easy answers but we dont want to learn. We want safety but we dont want to ask. We want pills but we dont want to read. Thats the real warning sign. 🌍
Jenny Salmingo
January 13, 2026 AT 03:20My mom moved here from Mexico and she didn’t understand any of the symbols. But she knew the word 'alcohol' because the pharmacy printed it in Spanish too. Simple. Clear. Human. We need more of that. Not more icons.
Lawver Stanton
January 14, 2026 AT 02:56Let me tell you about the time I got a prescription for gabapentin and the bottle had SEVEN warning stickers. One said 'avoid alcohol,' another said 'don't drive,' another said 'may cause dizziness,' another said 'take with food,' another said 'do not crush,' another said 'may interact with other meds,' and the last one said 'for external use only'-which was just a typo. The pharmacist didn't even notice. I called them. They said, 'Oh, that one's for a different patient.' I had to wait 20 minutes for a new bottle. This isn't healthcare. It's a game of Russian roulette with a printer.
Martin Viau
January 15, 2026 AT 08:20You think this is bad? Try getting a prescription in Canada. We have ONE national standard. Nine icons. Clear text. No chaos. Americans act like they invented medicine. Meanwhile, the rest of the world fixed this decades ago. Stop being so proud of your mess.
Urvi Patel
January 16, 2026 AT 00:14This post is so long I lost interest by the third paragraph. But I read the part about the dropper symbol. That’s insane. Why do we even have symbols if they mean nothing? Just write the words. In big letters. Done.
Joy Nickles
January 16, 2026 AT 16:12I got a pill that said 'do not crush' but the icon looked like a smashed tablet?? I was so confused I called my sister. She said 'maybe it means DO crush??' I didn't take it. I threw it out. Now I just Google everything. I don't trust no stinkin' stickers.
Emma Hooper
January 18, 2026 AT 05:56The real problem? We treat medicine like a puzzle instead of a lifeline. You wouldn’t drive a car without reading the manual. Why do it with your pills? Stop being a zombie. Ask. Read. Live. 🌟