Medication errors are one of the most common causes of preventable harm in home care. One in five people receiving home-based treatment experiences an adverse drug event - and most of these aren’t accidents. They’re the result of miscommunication, unclear labels, or forgotten supplements. If you’re managing multiple prescriptions, caring for someone with dementia, or just trying to keep track of what you’re taking and why, a personal medication safety plan isn’t optional. It’s your best defense.
Start with a Complete Medication List
Before you talk to your doctor or pharmacist, write down everything you take. Not just prescriptions. Include over-the-counter painkillers, vitamins, herbal teas, and supplements. People often leave these out because they think they’re "not real medicine." But that’s exactly when things go wrong. St. John’s Wort can cancel out antidepressants. Calcium supplements can interfere with thyroid meds. Even a daily gummy vitamin might cause a dangerous interaction. Use a simple notebook or a free app on your phone. Write the name of each medicine, the dose, how often you take it, and why your doctor prescribed it. If you don’t know the reason, write "unknown" - but make sure you ask at your next appointment. Don’t rely on memory. A 2023 study found that patients forget or misremember up to 40% of their medications when asked without a list.Verify Every Medication with Your Care Team
Bring your list to every appointment - doctor, pharmacist, even the physiotherapist. Don’t wait for them to ask. Say: "I’ve listed everything I’m taking. Can you check for interactions?" Pharmacists are trained to spot these. They’ll tell you if two drugs cancel each other out, or if one increases the risk of falling. Ask three key questions for every new prescription:- What is this for?
- What happens if I miss a dose?
- What side effects should I watch for?
Label Everything Clearly
Empty pill bottles are dangerous. If you can’t read the label, you can’t trust it. Even if you’ve been taking the same pill for years, your vision might change. Your memory might slip. That’s why every container - even the little blister packs - needs a clear label. Your label should include:- Your full name
- Medication name
- Dosage (e.g., 10mg)
- How often to take it (e.g., once daily at breakfast)
- Who prescribed it (doctor’s name)
- Emergency contact number
Store Medications Safely
Keep all medicines out of reach - not just from kids, but from confusion. A 2023 Reddit post from a caregiver in Bristol described how their mother kept heart pills next to her bed in an unlabeled bottle. She took one thinking it was her blood pressure medicine. It was a different drug. She ended up in A&E. Use a locked cabinet, a locked box, or even a small safe. If you live alone and worry about forgetting to take your meds, use a pill organizer with compartments for morning, afternoon, evening, and night. Fill it weekly. Set alarms on your phone. Put sticky notes on the mirror: "Take your diabetes pill after brushing your teeth." Never store pills in the bathroom. Heat and moisture ruin them. Keep them in a cool, dry place - a bedroom drawer or kitchen cabinet away from the sink.
Use a Pill Organizer and Daily Routine
A pill box isn’t just a convenience. It’s a safety tool. If you take eight pills a day, trying to remember which is which is a recipe for error. A seven-day pill box with AM/PM slots cuts that risk in half. Set up a routine. Take your meds at the same time every day - linked to habits you already do. After breakfast. Before bed. After brushing your teeth. Consistency reduces mistakes. If you have memory issues, ask a family member to help fill the box once a week. Or use a smart dispenser that beeps when it’s time and locks the next dose until the right hour. These aren’t fancy gadgets - they’re medical tools, like a walker or hearing aid.Schedule Regular Check-Ins
Medication needs change. Your kidneys slow down with age. A new condition might mean you need to stop one drug and start another. A drug that was fine last year might cause problems now. Set a calendar reminder: every three months, sit down with your GP or pharmacist and review your list. Bring your pill box. Show them what you’re actually taking - not what’s on paper. Ask: "Is everything still needed?" "Are there cheaper or safer options?" "Any new warnings?" If you feel off - more tired, confused, dizzy, nauseous - don’t wait for your next appointment. Call your care team. These could be signs of a bad interaction or overdose.Plan for Emergencies
Keep a printed copy of your medication list in your wallet, purse, or coat pocket. Also leave one taped to the inside of your fridge. If you collapse or are taken to hospital, paramedics and ER staff need to know what’s in your system. Don’t rely on your phone - it might be dead, lost, or locked. Include emergency contacts: your primary doctor, pharmacist, and a trusted family member. Add any allergies - not just "penicillin," but "causes rash, swelling, trouble breathing." Write down your most serious condition: "Type 2 diabetes," "heart failure," "severe dementia." If you’re at high risk - say, you take blood thinners or strong painkillers - give a copy to a neighbor or friend. Ask them to check in weekly. A simple text: "Did you take your meds today?" can prevent disaster.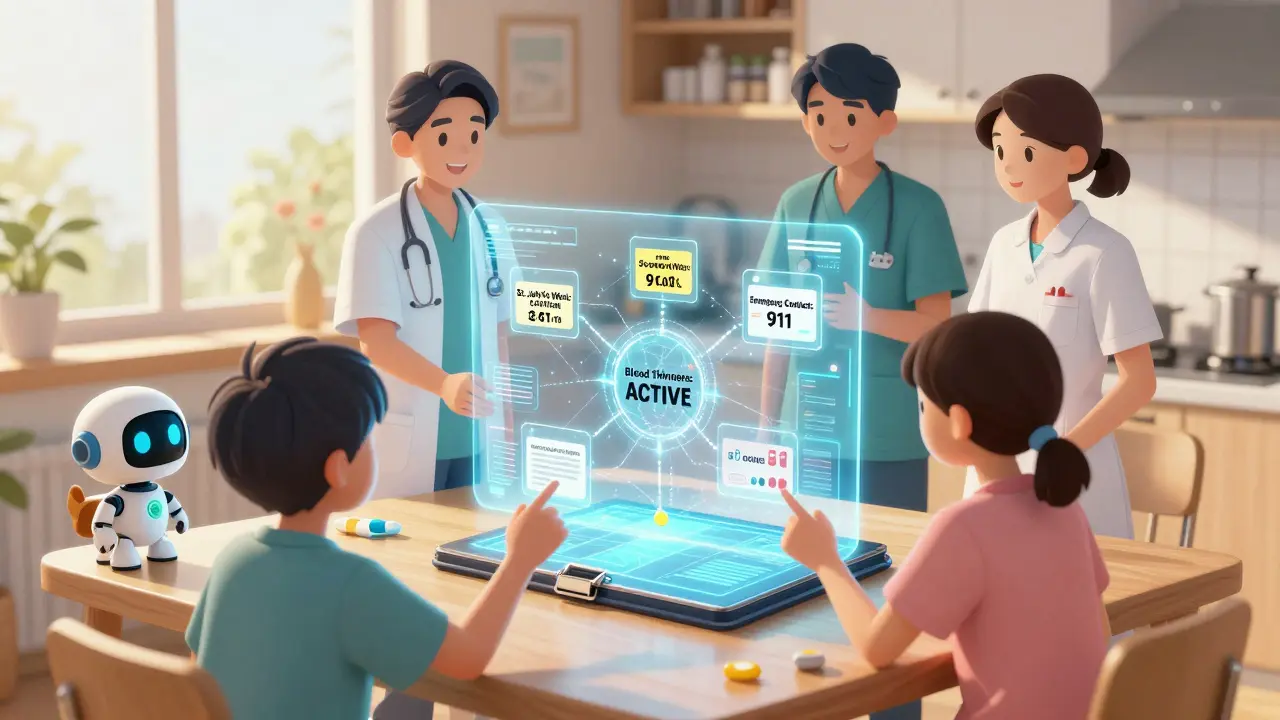
Involve Your Care Team as a Team
Your safety plan isn’t just yours. It’s yours and your care team’s. That means your GP, pharmacist, nurse, social worker, and family. Everyone needs the same information. Ask your doctor to send a copy of your updated list to your pharmacist. Ask your pharmacist to send updates to your GP. If you use a home care agency, make sure they get a copy too. Use a shared digital folder (like Google Drive) or a printed binder kept in a central place. If you’re seeing multiple specialists - cardiologist, neurologist, rheumatologist - ask one of them to be your "medication coordinator." They can help untangle overlapping prescriptions and flag conflicts.What If You Can’t Do It Alone?
If you have dementia, severe anxiety, depression, or physical limitations, you don’t have to manage this alone. Ask for help. It’s not weakness - it’s smart. Many communities offer free medication management services through local charities or public health programs. In Bristol, the Age UK outreach team can visit your home to help organize pills, check labels, and connect you with a pharmacist. If you have a family member or friend who’s reliable, give them access to your meds and a copy of your plan. Let them fill the pill box. Let them call your doctor with questions. You’re not giving up control - you’re building a safety net.Why This Works
This isn’t theory. It’s proven. Hospitals that use these exact steps see 50-60% fewer preventable drug errors. Patients who keep updated lists and use pill organizers are 70% less likely to be hospitalized for medication problems. The goal isn’t perfection. It’s reduction. One mistake can change your life. But with a plan, you’re not just surviving your meds - you’re in control of them.What if I forget to take my medication?
If you miss a dose, don’t double up unless your doctor says to. Most medications are safe if you skip one dose and return to your regular schedule. Keep a log of missed doses - write down when and why. Bring this to your next appointment. Some pills, like blood thinners or antibiotics, need strict timing. Ask your pharmacist which ones are critical.
Should I use a digital app for medication tracking?
Apps can help, especially with reminders. But they’re not foolproof. If you’re not tech-savvy, or if your phone dies, you’re left without a backup. Use apps as a supplement, not a replacement. Always keep a printed list. The most reliable systems combine technology with human oversight - like a daily phone call from a family member or a weekly check-in with a pharmacist.
Can I stop a medication if I feel better?
Never stop a prescribed medicine without talking to your doctor. Some drugs, like antidepressants or blood pressure pills, need to be tapered off slowly. Stopping suddenly can cause withdrawal, rebound high blood pressure, or even a heart attack. Even if you feel fine, the medication might be doing its job. Always ask before making changes.
How often should I update my medication list?
Update your list every time you start, stop, or change a dose - even if it’s a one-time antibiotic. At minimum, review it every three months with your GP or pharmacist. Keep a dated version. If you go to the hospital or ER, show them the most recent one.
What should I do if I notice a new side effect?
Write down the symptom, when it started, and what you were taking at the time. Call your pharmacist first - they can tell you if it’s a known side effect or something serious. If it’s severe - chest pain, trouble breathing, swelling, confusion - go to urgent care or call 111. Don’t wait. Side effects are signals, not annoyances.
Are herbal supplements really dangerous with prescription drugs?
Yes. Garlic, ginseng, ginger, and St. John’s Wort can interfere with blood thinners, antidepressants, and heart medications. Many people think "natural" means safe. It doesn’t. Always tell your doctor and pharmacist about every supplement you take - even if you think it’s harmless. They’ve seen the interactions. You haven’t.
What if my care team doesn’t take my concerns seriously?
You have the right to be heard. If you feel dismissed, ask for a second opinion. Request a medication review with your pharmacist - they’re often more available and trained specifically in drug safety. You can also contact Patient Advice and Liaison Service (PALS) at your local hospital. They help patients navigate concerns with care teams. Don’t give up. Your safety matters.

Radhika M
December 18, 2025 AT 05:42Simple list works best. I write everything on a notepad - pills, gummies, teas. Even the turmeric I take for knees. My pharmacist was shocked I even knew what I was on. She said most people forget half. Now I carry it in my purse. Life saver.
Don’t overcomplicate it. Just write it down. Then show it to someone.
That’s it.
Steven Lavoie
December 18, 2025 AT 17:27This is one of the most practical, human-centered guides I’ve seen on medication safety. As someone who’s worked with elderly patients across rural and urban settings in the U.S., I can say with confidence: the real breakthrough isn’t the tech - it’s the consistency. People don’t fail because they’re careless. They fail because systems don’t meet them where they are.
The labeling advice? Gold. I’ve seen patients take insulin thinking it was their blood pressure pill because the bottle had a faded label. No one meant for that to happen. But without clear, bold, written instructions - not abbreviations - it’s inevitable.
And the fridge copy? Brilliant. Emergency responders don’t have time to search phones. A printed list taped to the fridge is the quiet hero of home care.
Thank you for writing this. It’s not just advice - it’s a lifeline.
Anu radha
December 19, 2025 AT 13:40I help my aunt take her meds. She has dementia. We use a pill box with big labels and I set alarms on my phone for her. She forgets I’m helping - but she remembers the beeping. So it works.
She used to keep all her pills in a makeup bag. I cried when I saw it. Now everything’s in a locked drawer. We even put her emergency list in her shoebox with her photos. She knows that box. She’ll find it.
Small things. Big difference.
Jigar shah
December 19, 2025 AT 16:18Interesting that the post mentions St. John’s Wort specifically. I did a quick literature review last month - it interacts with over 60 common medications, including SSRIs, birth control, and even some statins. Yet most patients don’t consider it a ‘drug’ because it’s sold as a supplement.
Pharmacists know this. Doctors? Less so. That’s why the advice to bring your list to every appointment - even physio - is critical. You’re not being annoying. You’re preventing a hospitalization.
Also, the ‘don’t double up’ tip is vital. I’ve seen people take two doses because they thought they missed one. Then they end up in the ER with low blood pressure or liver stress.
Good post. Practical. No fluff.
Naomi Lopez
December 21, 2025 AT 13:59Ugh, another ‘medication safety’ guide. Honestly, if you can’t manage your own pills, maybe you shouldn’t be living alone. This is just enabling dependency. People need to take responsibility. I’m not saying don’t use pill organizers - I’m saying stop treating adults like children.
Also, why are we assuming everyone has a ‘care team’? What if you’re poor, alone, and on Medicare? This feels like a luxury checklist for people who have time and support.
Just saying.
Salome Perez
December 21, 2025 AT 15:09My heart swells reading this. Not because it’s perfect - but because it’s *human*. I’ve spent years working with older adults in Chicago, and I’ve seen too many stories like the one about the unlabeled heart pill next to the bed. It breaks my heart every time.
What’s beautiful here is how it doesn’t shame. It doesn’t say, ‘You’re failing.’ It says, ‘Here’s how we can help you succeed.’ That tone? That’s rare.
I’ve started handing out laminated medication list templates at our senior wellness fairs. People cry when they see their own meds written out - for the first time, they realize how much they’re juggling.
And yes - the fridge copy. Always the fridge copy. Paramedics look there first. I’ve seen it.
Thank you. This isn’t just advice. It’s dignity.
Jane Wei
December 23, 2025 AT 09:45My grandma used to take her blood pressure pill with coffee. Turns out coffee makes it less effective. She didn’t know. No one told her. Now I put her meds next to her toothbrush. Brush teeth → take pill. Simple.
Also, she calls me every morning at 8:15 to confirm she took it. I don’t answer. I just text back: ‘Good job.’ She loves that.
Small wins.
Jody Patrick
December 24, 2025 AT 03:53Americans are too soft. If you can’t manage your meds, you shouldn’t be left alone. This whole guide is overkill. Just take your pills. Stop making it a project.
Stop coddling people. Discipline is the answer.
End of story.
Philippa Skiadopoulou
December 24, 2025 AT 15:21Clarity is paramount. Labels must be legible, unambiguous, and permanent. Abbreviations are a liability. The phrase ‘once daily’ is superior to ‘QD.’
Emergency documentation must be physical. Digital systems fail. Power outages, device loss, forgotten passwords - all real.
Verification with pharmacists is non-negotiable. They are the last line of defense.
This framework is evidence-based. Implement it. Do not improvise.
- P.S. The Bristol case cited is not anecdotal. It is documented in the 2023 NHS safety bulletin.
Pawan Chaudhary
December 24, 2025 AT 18:50I’m 72 and I take 9 pills a day. I used to forget half of them. Then my son got me a pill box with alarms. Now I feel like a superhero.
People think getting older means giving up. Nah. It means getting smarter. This plan? It’s not about being old. It’s about being wise.
Keep going. You’re helping more than you know.