Every year, over 1.3 million people in the U.S. suffer injuries from medication errors. Many of these happen because doctors, pharmacists, or even patients miss dangerous combinations between prescription drugs, over-the-counter pills, and supplements. The good news? You don’t need to guess or flip through thick reference books anymore. Pharmacy apps now give you instant, accurate warnings about drug interactions - right on your phone.
Why Drug Interactions Matter
It’s not just about mixing two pills. A common cold medicine with antihistamines might make your blood pressure medication ineffective. A daily aspirin could turn dangerous when taken with certain blood thinners. Even natural supplements like St. John’s Wort or garlic pills can interfere with prescription drugs. The problem gets worse with age: nearly half of Americans over 65 take five or more medications daily. That’s a lot of chances for something to go wrong.
These aren’t rare edge cases. Studies show that 30-40% of clinically significant interactions go undetected by free or consumer-focused apps. That’s why professionals rely on trusted tools built for clinical use - not just quick searches.
How Pharmacy Apps Work
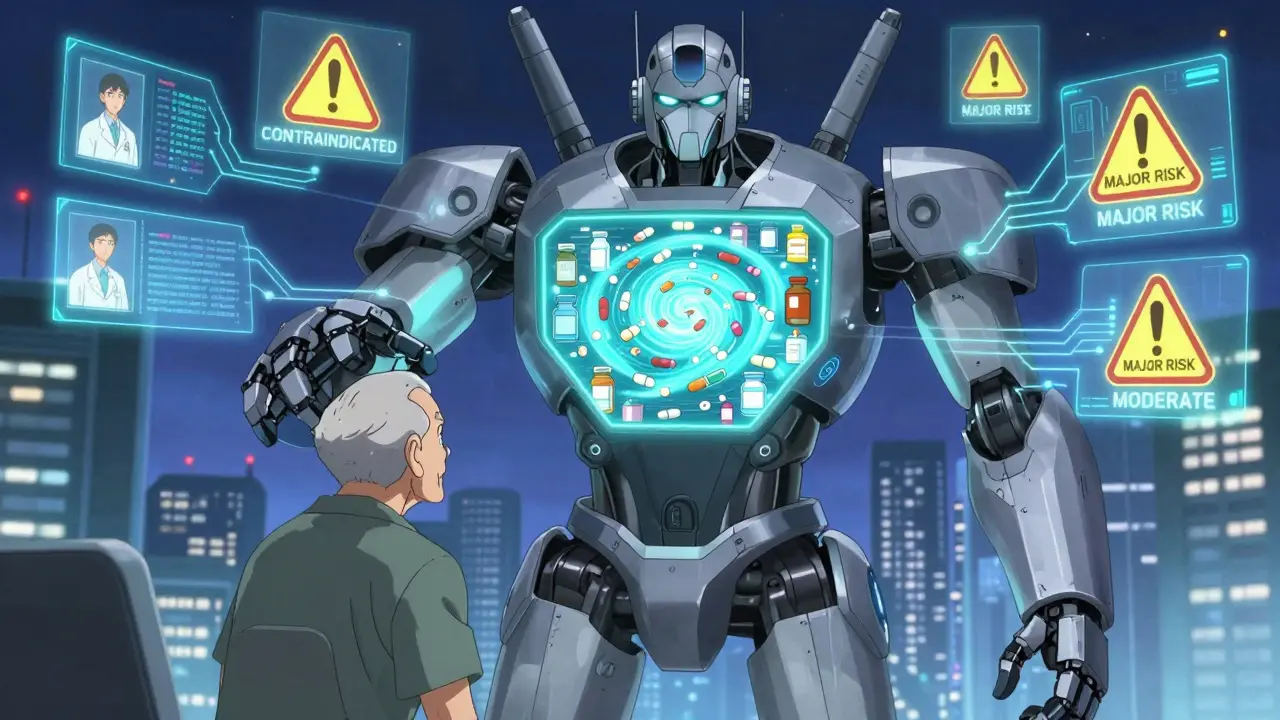
Modern pharmacy apps don’t just list side effects. They connect the dots between everything you’re taking - prescriptions, OTC meds, vitamins, even herbal teas. When you enter your full list, the app cross-references it against a database of thousands of known interactions. It doesn’t just say “possible interaction.” It tells you:
- Is this a contraindicated mix (never take together)?
- Is it a major risk (could cause organ damage or hospitalization)?
- Is it moderate (may need dose adjustment)?
- Or just minor (unlikely to cause harm)?
Besides checking interactions, many apps also help you identify pills by taking a photo, scan barcodes on bottles, or even using voice input to add medications. Some go further - offering overdose guidance, dosing reminders, and patient education sheets.
Top Pharmacy Apps Compared
Not all apps are created equal. Here’s how the leading options stack up based on real-world use by pharmacists and clinicians:
| App | Max Medications Checked | Offline Access | Free Version? | Key Strength | Limitations |
|---|---|---|---|---|---|
| Epocrates | 30 | Yes | Yes (limited) | Fastest interface, 92% pill ID accuracy | Slower with >20 meds; premium costs $50/month |
| Lexicomp | 50+ | Yes | No | Most comprehensive database, IV compatibility, pharmacogenomics | Steep learning curve; $199/year |
| UpToDate | 50+ | Yes | No | Overdose protocols, toxidrome info, clinical context | Expensive ($499+/year); better for institutions |
| Drugs.com | Unlimited | Yes | Yes | Free, FDA alerts, A-Z drug database | Ads interrupt checks; misses 30-40% of major interactions |
| Medscape | 30 | Yes | Yes | Great disease reference integration | Interaction feature locked behind paywall |
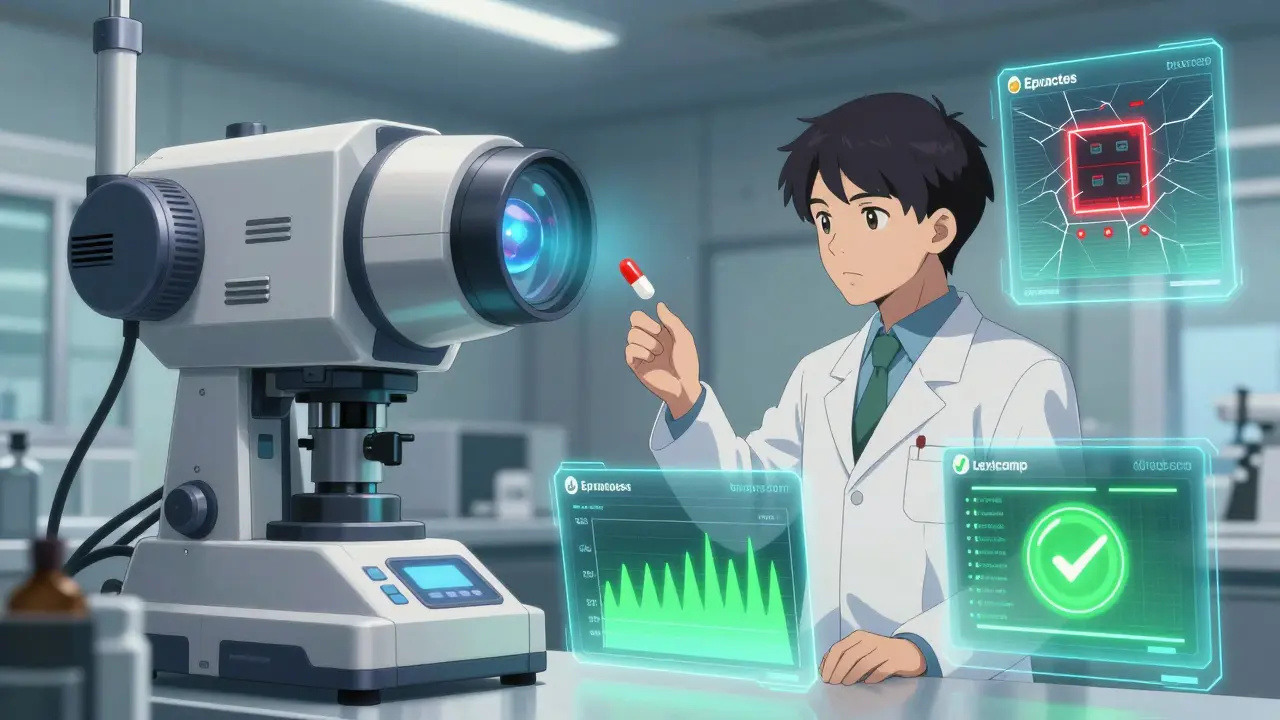
Professional-grade apps like Epocrates and Lexicomp catch 98.7% of serious interactions. Consumer apps like Drugs.com catch about 76%. That gap isn’t small - it’s life-or-death.
How to Use These Apps Effectively
Using the app is simple. Doing it right takes discipline. Follow this workflow:
- Add every medication - not just prescriptions. Include OTC painkillers, sleep aids, vitamins, herbal supplements, and even topical creams. Missing one item can hide a major risk.
- Use the camera or barcode scanner - if you’re unsure what a pill is, take a picture. Epocrates and others now use AI to match pill shapes, colors, and imprints with over 90% accuracy.
- Review the risk levels - don’t just glance at “moderate” or “minor.” Read the clinical notes. Some interactions only matter if you have kidney disease or are elderly.
- Double-check with a second app - Dr. Robert Johnson’s advice holds true: use Epocrates for speed, and Lexicomp or Micromedex for depth. Cross-referencing catches discrepancies.
- Document your check - write down the date, the app used, and what you found. This protects you legally and helps future providers.
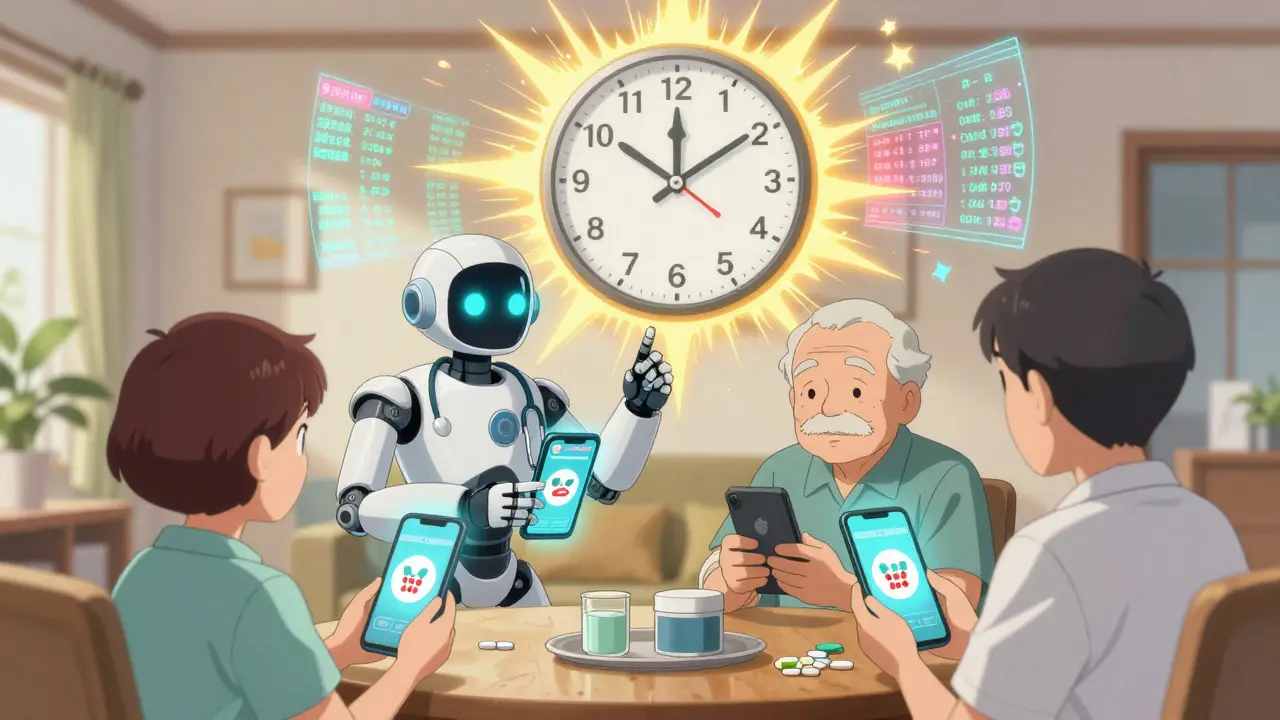
Pro tip: If you’re managing medications for an aging parent, use apps with caregiver sync features. Medisafe lets you add family members who get alerts if a new interaction is flagged.
What to Watch Out For
Even the best tools have blind spots. Here’s what you need to know:
- Free apps aren’t reliable - Studies show free tools miss up to 40% of dangerous interactions. Ads, limited databases, and outdated data make them risky.
- Severity ratings vary - A “major” interaction in one app might be “moderate” in another. A 2023 JAMA study found this happened in 28% of drug pairs. Always read the explanation, not just the label.
- Don’t trust AI predictions alone - New AI features (like Epocrates’ 2023 tool) estimate risk based on comorbidities. They’re helpful, but not replacements for clinical judgment.
- Update regularly - New drug interactions are discovered every week. Apps with automatic updates (like Lexicomp) are safer than ones that require manual downloads.
Who Should Use These Apps?
These aren’t just for doctors. Anyone managing multiple medications should use them:
- Patients on 5+ meds - Especially seniors. Polypharmacy is the #1 cause of preventable hospitalizations in older adults.
- Pharmacists and nurses - A 2023 survey found Epocrates reduced medication errors by 22% in hospitals that adopted it.
- Primary care providers - With CMS requiring interaction checks for Medicare Part D since 2022, this isn’t optional anymore.
- Family caregivers - Apps like Medisafe let you monitor a loved one’s meds remotely and get alerts if something’s wrong.
If you’re a patient, ask your pharmacist to show you how to use one. Most offer free training.
The Future of Drug Interaction Checking
The market is growing fast. The global medication management app industry hit $3.2 billion in 2023 and is projected to hit $8.7 billion by 2028. Why? Because the need is urgent.
New features are rolling out fast:
- AI-powered risk scoring - Apps now factor in age, kidney function, and liver health to predict interaction severity.
- AR pill identification - The latest updates let you point your phone at a pill and see its name, dose, and warnings overlaid in real time.
- Integration with EHRs - Apps like Lexicomp now sync with hospital records, so your doctor sees what you’re taking - even if you didn’t tell them.
But progress isn’t perfect. Discrepancies between databases still exist. That’s why experts agree: never rely on just one app. Use two. Always verify. And never skip checking - even if you’ve taken the same combo for years.
Final Thoughts
Drug interactions don’t care if you’re busy, tired, or confident. They don’t care if you’ve been on a medication for 10 years. A new supplement, a change in dosage, or even a different brand of generic can trigger a silent danger.
Pharmacy apps are the easiest, fastest, and most reliable way to prevent harm. You don’t need to be a doctor to use them. You just need to be careful. Start today - add your medications, check for interactions, and make it part of your routine. It could save your life - or someone else’s.