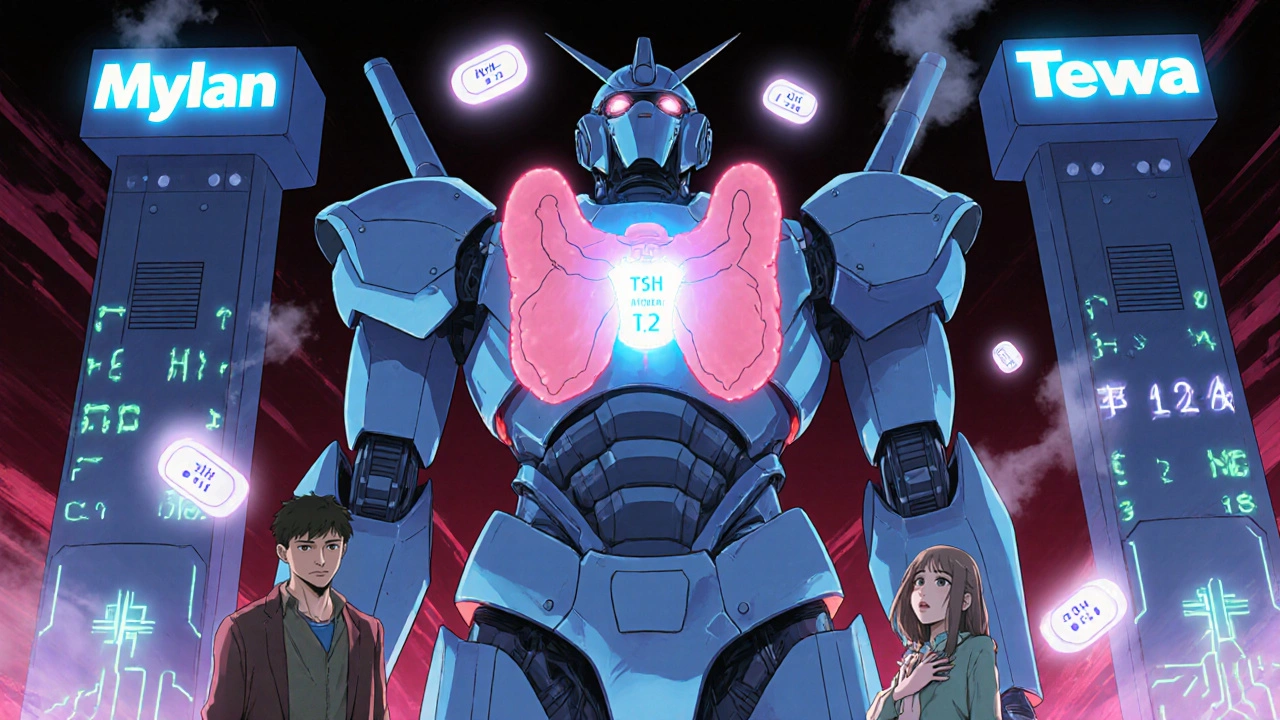
Switching between different generic versions of levothyroxine is common - and often unavoidable. With over 89% of prescriptions in the U.S. now filled with generics, most people on thyroid hormone replacement are taking a product made by Mylan, Teva, Pfizer, or Sandoz. But here’s the real question: do you need to get your TSH checked every time your pharmacy switches your pill?
Why This Matters More Than You Think
Levothyroxine isn’t just any pill. It’s a narrow therapeutic index (NTI) drug, meaning tiny changes in blood levels can throw your whole system off. Too little, and you feel exhausted, cold, and gain weight. Too much, and your heart races, you lose weight without trying, and your bones weaken over time. Your TSH level - the hormone your pituitary gland releases to signal your thyroid - is the most reliable way to know if your dose is right. Most adults should stay between 0.4 and 4.0 mIU/L. For older people or those with heart issues, the upper limit might stretch to 6.0 mIU/L.The FDA says all approved generics are interchangeable. They meet strict bioequivalence rules: the amount of drug absorbed must fall within 80-125% of the brand-name version. That sounds solid. But here’s the catch: some patients report feeling worse after a switch. Fatigue. Palpitations. Weight shifts. And sometimes, their TSH jumps from 1.8 to 7.2 - a clear sign their body isn’t handling the change.
What the Science Actually Shows
A major 2022 study published in JAMA Internal Medicine looked at over 15,000 people who switched between generic levothyroxine products. The results? No meaningful difference in TSH levels between those who switched and those who didn’t. The average TSH was 2.7 mIU/L in both groups. That’s not a fluke - it was a large, well-designed study using real-world data from Kaiser Permanente.Another study of 2,780 matched patient pairs found that 64% of switchers stayed within normal TSH range, compared to 64% of non-switchers. The chance of ending up with a dangerously high or low TSH was virtually identical - 10% either way. These findings led the FDA to update its labeling in January 2024: “For most patients, switching between different levothyroxine products does not require additional TSH monitoring beyond routine follow-up.”
But not everyone agrees. The European Medicines Agency still recommends checking TSH 6-8 weeks after any switch. And back in 2014, the American Thyroid Association and American Association of Clinical Endocrinologists advised routine testing after every change. Why the shift? Because the old advice was based on small studies and patient anecdotes. Now, we have real-world data from millions of prescriptions.
Who Really Needs a TSH Check After a Switch?
If you’re not in one of these groups, you probably don’t need extra testing:- You’re stable on your current dose
- You have no heart problems
- You’re not pregnant or planning to be
- You’ve never had abnormal TSH levels after a switch before
But if you fall into one of these higher-risk categories, get your TSH checked 6-8 weeks after switching:
- Thyroid cancer survivors - They often need tighter control, with TSH targets below 0.1 or even undetectable levels.
- Pregnant women - Thyroid needs change dramatically during pregnancy. Even a small change in levothyroxine can affect fetal brain development.
- People with severe heart disease - Too much thyroid hormone can trigger arrhythmias or angina.
- Those who’ve had symptoms after past switches - If your TSH jumped before, it might happen again.
- Patients on high doses (>100 mcg daily) - Some studies suggest they’re more sensitive to formulation differences.
The UK’s Commission on Human Medicines put it well: “A small proportion of patients report symptoms when their levothyroxine is changed.” That’s about 8-12% of users. For them, consistency matters. For the other 88-92%, it doesn’t.

What Symptoms Should You Watch For?
If you switch brands and start feeling off, don’t ignore it. The most common complaints reported to the UK’s Yellow Card system include:- Fatigue (327 cases)
- Palpitations (289 cases)
- Weight gain or loss (215 cases)
- Brain fog
- Depression or anxiety
These aren’t “all in your head.” They’re real signs your thyroid hormone levels might be off. If you notice any of these within 4-8 weeks of a switch, ask your doctor for a TSH test. Don’t wait for your next routine checkup.
Why Do Some People React and Others Don’t?
It’s not random. Research is starting to pinpoint why a few people are sensitive:- Excipient intolerance - Some generics use different fillers like lactose, corn starch, or dyes. A 2022 study found 1.7% of patients had reactions tied to these inactive ingredients.
- DIO2 gene variants - This gene helps convert T4 to active T3. About 0.8% of people have a variant that makes them less efficient at this. For them, even small changes in absorption can matter.
- Thyroid receptor sensitivity - Some people’s cells respond differently to thyroid hormone. This affects about 2.1% of the population.
- Very low thyroid reserve - If your thyroid was destroyed by surgery or radiation, your body has zero backup. You’re more vulnerable to absorption changes.
If you’ve had problems before, your doctor might consider keeping you on one brand - even if it costs more. Some pharmacies can special-order a specific generic. It’s not ideal, but for those few, it’s necessary.

The Cost of Consistency
Brand-name Synthroid still costs around $45 for a 90-day supply. Generic levothyroxine? About $4.37. That’s a 90% savings. In the U.S. alone, switching to generics saves $2.1 billion a year. Pharmacy benefit managers push generics because they work - for most people.But if you’re one of the 8-12% who reacts, that savings comes at a cost: extra doctor visits, lab tests, and possibly higher doses to compensate. That’s why some clinics now track patient-reported outcomes. If you say you feel worse after a switch, they don’t just shrug. They test.
What Should You Do?
Here’s a simple action plan:- If you’re stable and have no risk factors - no need to test after a switch. Stick to your regular 6-12 month TSH check.
- If you’re high-risk (cancer, pregnancy, heart disease) - get a TSH test 6-8 weeks after any change.
- If you feel worse after switching - get tested. Don’t wait. Symptoms matter.
- If you’ve had a bad reaction before - ask your doctor to prescribe a specific generic brand. Many pharmacies can accommodate this.
- If your pharmacy switches your pill without telling you - keep a record. Note the name on the bottle. If symptoms appear, you’ll know what changed.
There’s no one-size-fits-all answer. But the evidence is clear: for most people, switching generics is safe. For a small group, it’s not. The key is knowing which group you’re in.
What’s Next?
The American Thyroid Association is updating its guidelines in late 2024. Expect them to align more closely with the FDA’s position: routine monitoring isn’t needed for most. But they’ll still recommend it for high-risk patients.Future research might even include genetic testing to identify who’s sensitive before they ever switch. For now, the best tool is your own body. Pay attention. Speak up. And if something feels off - get your TSH checked. It’s simple, cheap, and could prevent a lot of unnecessary suffering.
Do I need to get my TSH checked every time my pharmacy switches my levothyroxine brand?
No, not for most people. If you’re stable, have no heart issues, aren’t pregnant, and haven’t had problems after past switches, routine TSH testing isn’t needed. The FDA and recent large studies show no significant difference in TSH levels after switching between approved generics. Only check if you feel worse or if you’re in a high-risk group.
Which generic levothyroxine brands are most commonly used?
The four largest manufacturers in the U.S. are Mylan (32% market share), Teva (28%), Pfizer (22%), and Sandoz (18%). These make up nearly 100% of the generic market. Their products are all FDA-approved and bioequivalent, but they use different inactive ingredients, which can affect a small number of people.
Can switching levothyroxine brands cause weight gain?
Yes, in some cases. If the switch causes your TSH to rise (meaning you’re under-treated), your metabolism slows down, leading to weight gain. If your TSH drops too low (over-treated), you might lose weight. This isn’t common - but it happens. If you notice unexplained weight changes after switching, get your TSH tested.
Why do some doctors still recommend checking TSH after every switch?
Some doctors follow older guidelines from 2014, which advised caution due to limited data. Others have seen patients react badly and prefer to err on the side of caution. But new evidence from large real-world studies shows that routine testing isn’t necessary for most. The medical community is shifting toward evidence-based practice - not fear-based.
Is it safe to switch between generics if I have Hashimoto’s?
Yes, for most people with Hashimoto’s. Hashimoto’s itself doesn’t make you more sensitive to formulation changes - but your body’s response to hormone levels does. If you’ve had symptoms after past switches, or if your TSH has been unstable, then monitor closely. Otherwise, no extra testing is needed. Many people with Hashimoto’s switch generics without issue.
What should I do if I suspect my new generic is making me feel worse?
First, check the name of the new product on your prescription bottle. Then, schedule a TSH test within 4-8 weeks. If your TSH is abnormal, your doctor may switch you back to your previous brand or adjust your dose. Keep a symptom journal - noting fatigue, heart rate, weight, and mood - to help your doctor see patterns.

Logan Romine
November 22, 2025 AT 02:32So let me get this straight - we’re trusting a pill that costs $4.37 to keep my metabolism from turning into a sluggish sloth? 🤡 I’ll believe it when I see the FDA’s ‘levothyroxine compatibility chart’ with emoji ratings. 📊💖
Chris Vere
November 22, 2025 AT 09:44The data presented here is compelling and reflects a shift toward evidence-based practice. While individual variability exists, population-level outcomes suggest that routine monitoring after generic switches is not universally required. This aligns with principles of rational pharmacotherapy and resource stewardship.
Pravin Manani
November 23, 2025 AT 15:26The bioequivalence thresholds of 80-125% are statistically sound, but the pharmacodynamic heterogeneity in NTI drugs like levothyroxine can’t be fully captured by AUC and Cmax alone. The DIO2 polymorphisms and excipient sensitivities are underappreciated in population studies - they’re not noise, they’re signal. We need phenotyping, not just genotyping, in clinical practice.
Mark Kahn
November 25, 2025 AT 04:48Hey, if you’re feeling off after a switch - don’t panic, but don’t ignore it either. Your body’s talking. A simple TSH test is like a quick checkup for your thyroid. 10 minutes, $20, peace of mind. You’ve got this 💪
Leo Tamisch
November 26, 2025 AT 23:39Ah yes, the FDA’s ‘trust us’ pamphlet. Meanwhile, real people are out here Googling ‘why do I feel like a zombie after my pharmacy switched my pill?’ 🤦♂️ The science says ‘it’s fine’ - but the lived experience says ‘this isn’t a toaster, it’s my metabolism.’
Daisy L
November 28, 2025 AT 08:58I’m sorry, but this is a total betrayal of American patients!!! We’ve been sold out by Big Pharma and Big Pharmacy for decades!! $4.37?!?! That’s not medicine - that’s a discount coupon for your soul!! I’ve been on the same generic since 2018 - and I’ve never felt better!! WHY ARE THEY DOING THIS TO US?!?!
Anne Nylander
November 29, 2025 AT 11:24if you switch pills and feel weird? just get your tsh checked!! its so easy!! dont wait!! your body knows!! and if you cant afford it? ask your doc for a coupon!! they can help!! you’re not alone!! 💕
Franck Emma
November 30, 2025 AT 11:15I switched brands last month. My heart’s been racing. I can’t sleep. I cried in the shower. My cat left me. It’s not me. It’s the pill.
Noah Fitzsimmons
December 1, 2025 AT 09:27Oh wow, so you’re telling me that the FDA says it’s fine, but you still feel like crap? Maybe you’re just lazy? Or maybe you’re one of those people who think their body is a special snowflake? 🤭
Eliza Oakes
December 1, 2025 AT 23:27Ohhh so now we’re supposed to believe the FDA over our own bodies? After the opioid crisis? After Vioxx? After the 2008 financial collapse? I’m sorry, but I don’t trust a system that lets a $4 pill replace my $45 brand and then tells me I’m being dramatic. This is gaslighting with a prescription pad.
Clifford Temple
December 3, 2025 AT 03:35This country is falling apart because we’re letting foreign manufacturers make our life-saving meds. My grandfather fought in Korea so we could have American-made pills. Now we’re giving our health to China and India for a buck. Shame on you.
Corra Hathaway
December 3, 2025 AT 08:54I switched to a new generic and felt like a ghost for two weeks 😅 but then I got my TSH checked - turned out I was underdosed. My doc adjusted it and now I’m back to running marathons 🏃♀️💖 Don’t ignore your body - it’s your best alarm system!
Shawn Sakura
December 3, 2025 AT 18:04I have been on levothyroxine for 18 years. I switched generics 7 times. Only once did I feel off. Got tested. TSH was 5.8. Doc adjusted. Back to normal. The system works. For most. Be patient. Be informed. You are not alone. 🙏
Paula Jane Butterfield
December 4, 2025 AT 19:22As a nurse who’s worked with thyroid patients for 22 years, I’ve seen everything. Some people are fine with any generic. Others? They need the same one forever. I always ask: ‘Have you felt different since your last refill?’ If yes - test. Simple. No shame. No stigma. Your health isn’t a cost center.
Swati Jain
December 6, 2025 AT 14:11The DIO2 variant prevalence in South Asian populations is ~1.9%, slightly higher than global average. This means that in places like India, where levothyroxine access is expanding rapidly, we need to build in phenotypic screening protocols - not just assume bioequivalence equals clinical equivalence. We’re not just patients; we’re data points with ancestry.