Pediatric Weight Management: Practical Strategies for Healthy Child Growth
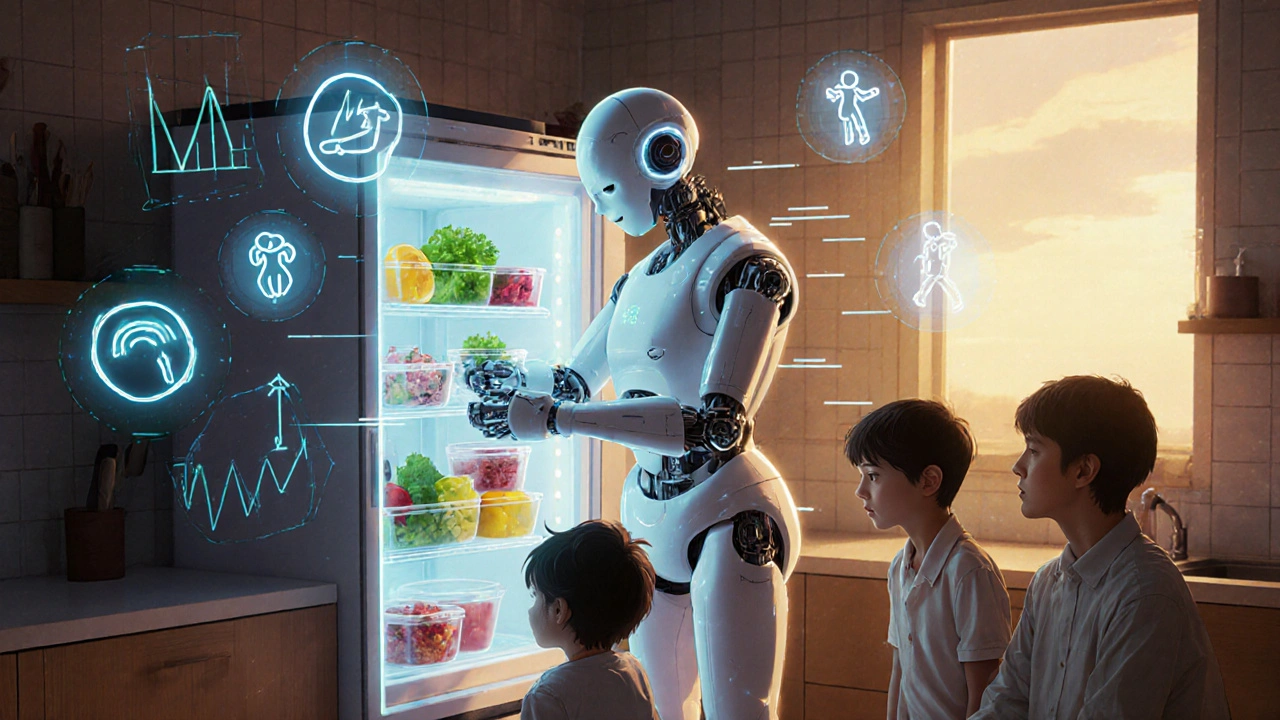
When we talk about pediatric weight management, the process of helping children maintain a healthy weight through balanced nutrition, physical activity, and behavioral support. Also known as childhood weight management, it’s not about restricting food or pushing kids to lose weight fast—it’s about building habits that support lifelong health. Many parents worry when their child gains weight, but the real goal isn’t a number on the scale. It’s whether the child is growing normally, has energy for play, sleeps well, and doesn’t have signs of metabolic stress like high blood pressure or insulin resistance.
Childhood obesity, a condition where excess body fat negatively affects a child’s health. Also known as pediatric obesity, it’s not just a cosmetic concern—it’s linked to early signs of heart disease, type 2 diabetes, and sleep apnea. And it’s not caused by laziness or bad parenting. It’s often tied to family routines, access to healthy food, screen time, sleep patterns, and even stress. The good news? Small, consistent changes make a big difference. Kids who eat more vegetables, drink water instead of soda, move daily, and get enough sleep often see natural improvements—even without drastic dieting.
Child nutrition, the practice of providing balanced, age-appropriate meals that support growth and development. Also known as children’s dietary needs, it’s the foundation of healthy weight. Forget counting calories for kids. Focus on whole foods: fruits, veggies, lean proteins, whole grains. Skip processed snacks, sugary drinks, and fast food. Portion sizes matter too—kids don’t need adult-sized meals. And don’t use food as a reward or punishment. That creates unhealthy relationships with eating.
BMI in children, a tool doctors use to track weight relative to height and age, adjusted for gender and growth patterns. Also known as childhood BMI percentiles, it’s not a diagnosis, but a flag. If your child is in the 85th percentile or higher, it doesn’t mean they’re unhealthy—but it does mean it’s time to check in with a doctor. They’ll look at growth trends over time, family history, activity levels, and lab markers like cholesterol or blood sugar. Don’t rely on apps or online calculators. Pediatric BMI is different from adult BMI, and only trained professionals should interpret it.
What you’ll find in the posts below isn’t a list of fad diets or quick fixes. It’s real, practical advice from trusted sources—like how metabolic syndrome shows up in kids, why certain medications can affect weight, how to read food labels for family meals, and what to do when a child’s weight starts to climb. These aren’t theoretical ideas. They’re tools used by doctors, dietitians, and parents who’ve been there. You don’t need to be perfect. You just need to be consistent. Start with one change. Maybe it’s swapping juice for water at dinner. Or taking a walk after school instead of turning on the TV. Small steps lead to big results—and they stick.
- November
24
2025 - 5
Childhood Obesity Prevention and Family-Based Treatment: What Works Now
Family-based behavioral treatment is the most effective way to prevent and treat childhood obesity. Learn how the Stoplight Diet, daily activity, and parent-led behavior change lead to lasting results for the whole family.
Read More