Phosphate Binders: Understanding Their Role in Kidney Health
When dealing with phosphate binders, medications that attach to dietary phosphate in the gut and prevent its absorption, you’re looking at a key tool for controlling serum phosphorus. Also known as phosphate binders, they are essential for people whose kidneys can’t filter phosphate efficiently. Chronic kidney disease often leads to hyperphosphatemia, a buildup of phosphorus that can cause bone and cardiovascular problems. To keep things in balance, many patients on dialysis rely on these agents. One popular non‑calcium option is sevelamer, which also helps lower LDL cholesterol. Together, these elements form a network where phosphate binders reduce serum phosphorus, chronic kidney disease creates the need, and dialysis patients benefit most.
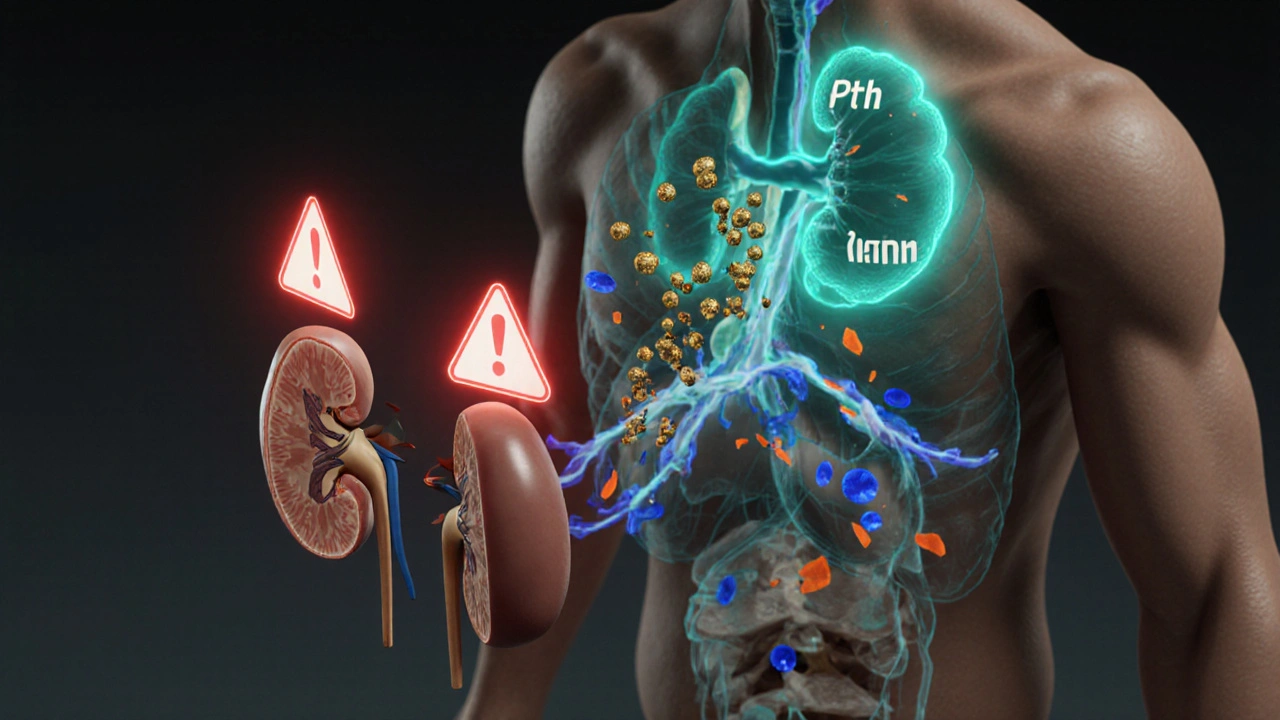
Why does phosphate build up in the first place? In healthy kidneys, excess phosphate is filtered out, but once kidney function drops below 15% of normal, the regulation fails. This failure triggers hyperphosphatemia, which activates parathyroid hormone and forces calcium out of bones, leading to renal osteodystrophy. The situation worsens when patients consume high‑phosphate foods like processed meats and sodas. That’s where phosphate binders step in: they act like a sponge in the gastrointestinal tract, latching onto phosphate particles and escorting them out of the body in stool. By doing so, they break the link between high phosphate and bone disease, and also protect blood vessels from calcification.
There are several classes of phosphate binders, each with its own pros and cons. Calcium‑based binders, such as calcium acetate and calcium carbonate, are affordable and work well for many, but they can raise calcium levels and increase the risk of vascular calcification, especially in patients already prone to calcium overload. Sevelamer, a polymer resin, avoids adding extra calcium and even lowers LDL cholesterol, making it a favorite for those with cardiovascular concerns. Lanthanum carbonate is another non‑calcium option; it’s very effective at low doses but can be pricey and may cause gastrointestinal side effects. Choosing the right binder depends on a patient’s overall health, lab results, and dietary habits.
Monitoring is just as important as picking the right binder. Regular blood tests for serum phosphorus, calcium, and PTH guide dosage adjustments. Most clinicians start patients on a low dose and increase gradually until phosphorus falls within the target range (usually 3.5–5.5 mg/dL). It’s also crucial to coordinate binder timing with meals—taking the binder with each main meal and snack maximizes phosphate capture. Missing doses or taking them without food reduces effectiveness and can lead to spikes in phosphorus levels.
Beyond the medication itself, diet plays a supportive role. Cutting down on processed foods, limiting dairy if calcium intake is already high, and choosing fresh fruits, vegetables, and lean proteins helps keep phosphate intake low. Some patients find it helpful to use a phosphate‑content calculator or work with a renal dietitian to track hidden sources in sauces, dressings, and even certain medications that contain phosphate buffers.
For patients on dialysis, the timing of binder administration can be synced with treatment schedules. Peritoneal dialysis patients often take binders with each exchange, while hemodialysis patients may benefit from a nighttime dose to cover the long interdialytic interval. Adjustments may be needed on days when dialysis frequency changes, such as during holidays or travel.
Now that you’ve got a clear picture of what phosphate binders do, how they fit into kidney disease management, and the factors that influence their use, you’re ready to explore the detailed guides below. From practical tips on choosing the right binder to in‑depth comparisons of calcium‑based versus non‑calcium options, the upcoming articles will give you actionable insights to keep your phosphorus levels in check.
- October
17
2025 - 5
Secondary Hyperparathyroidism and GI Problems: What’s the Link?
Explore how secondary hyperparathyroidism triggers nausea, constipation, and other gut problems, and learn practical steps to manage both the hormonal disorder and digestive health.
Read More