Symptom Risk Assessment Tool
How This Tool Works
This tool helps you assess infection risk based on your immunosuppressant medication and symptoms. Remember: immunocompromised patients often experience atypical symptoms like fatigue or mild rash without fever. Select your medication type and symptoms to get personalized risk assessment.
Risk Assessment Result
When your immune system is weakened-whether from cancer treatment, an organ transplant, or an autoimmune disease like rheumatoid arthritis or lupus-taking medication becomes a high-stakes balancing act. What helps control your condition might also leave you dangerously exposed to infections, some of which can turn life-threatening without warning. This isn’t just theoretical. Around 24 million Americans live with autoimmune diseases that often require immunosuppressants, and millions more are on these drugs after transplants or chemotherapy. The risks aren’t the same for everyone, and they don’t always show up the way you’d expect.
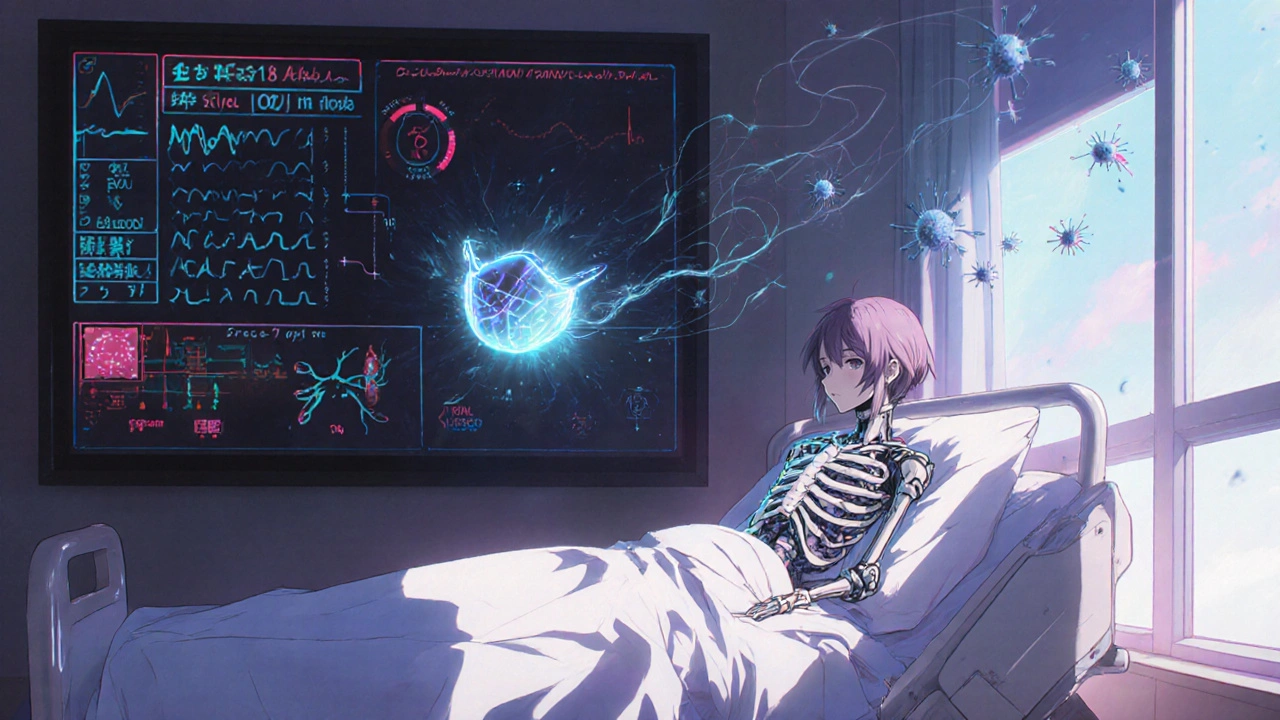
What Does ‘Immunocompromised’ Really Mean?
Being immunocompromised means your body’s defense system isn’t working the way it should. You might not get sick more often, but when you do, it’s harder to fight off. Infections can spread faster, last longer, and hide behind symptoms that look like something else. A fever might never show up. A cough might be mild. A rash might be the only sign of something serious. This isn’t just about being "weak". It’s about how specific drugs shut down parts of your immune system. Corticosteroids like prednisone reduce inflammation-and immune activity-by suppressing white blood cells. Methotrexate slows down the immune response by targeting rapidly dividing cells. Biologics like adalimumab (Humira) block specific proteins that trigger inflammation, but they also remove key signals your body uses to fight off bacteria and viruses. The problem? These drugs don’t just turn off the bad parts of your immune system. They turn off the good ones too.The Real Infection Risks by Drug Type
Not all immunosuppressants are created equal. Some carry higher risks than others, and those risks change depending on how long you’ve been on them and how much you’re taking.- Corticosteroids (prednisone, dexamethasone): Doses above 20mg per day of prednisone equivalent increase infection risk by 60% compared to placebo. Even short courses (over two weeks) can do it. What’s worse? They mask fever and other classic signs of infection. You might have pneumonia and feel only a little tired.
- Methotrexate: Used for rheumatoid arthritis and psoriasis, it causes fatigue, nausea, and mouth sores in about half of patients. But the real danger is liver and bone marrow suppression. Monthly blood tests are required because low white blood cell counts can sneak up without symptoms.
- Azathioprine: This drug lowers lymphocytes and can cause severe leukopenia. Patients on azathioprine are at higher risk for bacterial infections, hepatitis B reactivation, and rare but deadly conditions like PML (progressive multifocal leukoencephalopathy) caused by the JC virus.
- Biologics (TNF inhibitors, IL-6 blockers): These are the most powerful-and the riskiest. Studies show they’re significantly more likely to cause serious infections than older drugs like methotrexate. Herpes zoster (shingles) reactivation is common. Some patients get tuberculosis or fungal infections they never had before.
- Calcineurin inhibitors (cyclosporine, tacrolimus): Used after transplants, they increase risk of viral infections like CMV, EBV, and BK virus, which can damage kidneys or cause brain inflammation.
- Chemotherapy drugs (cyclophosphamide, paclitaxel): These aren’t just for cancer. They wipe out immune cells across the board. Patients on chemo are often neutropenic-meaning their body has almost no infection-fighting white blood cells.
Combining Drugs Makes Risks Worse
Many patients take more than one immunosuppressant. A transplant patient might be on tacrolimus, mycophenolate, and prednisone. Someone with severe lupus might get rituximab plus low-dose steroids. This isn’t always avoidable-but it’s dangerous. Research shows the combination of steroids and other immunosuppressants doesn’t just add risk-it multiplies it. One study found that patients on triple therapy had nearly three times the risk of serious infection compared to those on a single drug. And because each drug suppresses a different part of the immune system, your body loses multiple layers of defense at once. This is why doctors monitor blood counts, liver enzymes, and kidney function so closely. A drop in neutrophils might mean you’re one cold away from sepsis.
Atypical Symptoms: The Silent Danger
One of the most dangerous myths is that if you don’t have a fever, you’re fine. In immunocompromised patients, that’s often not true. Corticosteroids blunt your body’s ability to raise a fever. A person with pneumonia might only feel slightly out of breath. Someone with a urinary tract infection might just be more tired than usual. A skin infection might look like a simple rash. A headache could be meningitis. Doctors call this "masked infection." It’s why patients on long-term immunosuppressants are told to treat even minor symptoms seriously. If you feel off-even a little-get checked. Don’t wait. Don’t assume it’s just the medication.Vaccines, Masks, and Everyday Protection
You can’t stop taking your meds. But you can protect yourself.- Vaccines: Get them before starting immunosuppressants if possible. Flu shots, pneumococcal vaccines, and hepatitis B vaccines are critical. Avoid live vaccines (like MMR or shingles vaccine) once you’re on these drugs-they can cause the disease they’re meant to prevent.
- Handwashing: Wash for at least 20 seconds. Scrub between fingers, under nails, and up to your wrists. Use hand sanitizer when soap isn’t available.
- Masks: Wear one in crowded places, especially during flu season or if there’s a local outbreak. The CDC recommends this for immunocompromised people even when it’s not required for others.
- Wound care: Even a small cut can become infected. Clean it immediately, apply antibiotic ointment, and cover it.
- Vector-borne diseases: Mosquitoes and ticks carry diseases like West Nile, Lyme, and Rocky Mountain spotted fever. Immunocompromised people are more likely to get severely ill from these. Use repellent, wear long sleeves, and check for ticks after being outdoors.
What Patients Are Really Saying
Online communities are full of real stories. In r/RheumatoidArthritis, one user wrote: "I got shingles on my face while on Humira. I thought it was a bug bite. By the time I went to the ER, I was losing vision in one eye." Another said: "I lost 15 pounds in two weeks from nausea on methotrexate. But my joints stopped hurting. I’d do it again." On r/Transplant, someone shared: "Tacrolimus saved my life after my kidney transplant. But I’ve been hospitalized twice for pneumonia. My doctor says I’m lucky I didn’t die. I now carry an emergency card in my wallet that says I’m immunocompromised." These aren’t rare cases. They’re common. And they’re why many patients feel caught between two fears: the disease that’s killing them slowly, and the drugs that might kill them fast.Monitoring and Personalized Care
Regular blood tests aren’t optional. They’re lifesaving. For methotrexate, monthly CBC and liver tests are standard during the first year. For biologics, doctors often check for latent TB before starting. For transplant patients, viral load tests for CMV and EBV are routine. The future is moving toward personalized dosing. Some hospitals now use pharmacogenomic testing to predict how a patient will metabolize drugs like azathioprine. Others are developing biomarkers to predict infection risk before it happens-so you don’t have to wait for a fever to appear. And while early in the pandemic, everyone assumed immunosuppressed patients would die from COVID-19, Johns Hopkins found something surprising: their outcomes were often no worse than healthy people’s. Why? Maybe because their immune systems weren’t overreacting. Maybe because they were more careful. Or maybe because the virus itself behaves differently in suppressed bodies. The answer isn’t clear yet-but it shows we still have a lot to learn.The Bigger Picture
The number of people on immunosuppressants is rising. Autoimmune diseases are more common than ever. Antibiotic resistance is growing. The World Health Organization warns that drug-resistant infections could kill 10 million people a year by 2050-and immunocompromised patients will be hit hardest. This isn’t just about taking pills. It’s about living with constant awareness. Knowing your drug’s risks. Recognizing subtle symptoms. Asking for help before it’s too late. Talking to your doctor-not just about your disease, but about your life. You’re not just a patient. You’re someone managing a complex, high-risk treatment. And you deserve to know exactly what you’re up against.Can immunosuppressants cause cancer?
Yes, some immunosuppressants increase cancer risk, especially skin cancer and lymphoma. Long-term use of drugs like azathioprine and cyclosporine is linked to higher rates of non-melanoma skin cancer. That’s why regular skin checks are part of standard care. The FDA requires black box warnings for many of these drugs because of this risk. But the benefit of controlling a life-threatening autoimmune disease often outweighs the long-term cancer risk-especially when monitored closely.
Do I need to avoid people if I’m immunocompromised?
You don’t need to isolate yourself, but you should be smart. Avoid close contact with people who are sick. Ask visitors to wash their hands before coming in. Skip large crowds during flu season or if there’s a known outbreak. Wearing a mask in busy places like airports or hospitals is a simple, effective step. Many immunocompromised people find that with these precautions, they can still work, travel, and spend time with family safely.
What should I do if I think I’m getting sick?
Don’t wait. Call your doctor immediately-even if you only have a mild fever, cough, or feeling unusually tired. Don’t try to tough it out. Infections in immunocompromised patients can turn serious in hours. Your doctor may order blood tests, a chest X-ray, or start antibiotics before symptoms worsen. Keep a list of your medications and dosages handy for emergencies.
Can I still get the flu shot or COVID booster?
Yes, and you should. Inactivated vaccines (like the flu shot and mRNA COVID boosters) are safe and recommended. They won’t give you the disease. But they might not work as well as they do in healthy people. That’s why extra doses are often advised-for example, the CDC recommends additional COVID boosters for immunocompromised individuals. Talk to your doctor about your vaccination schedule. Don’t assume one shot is enough.
Is there a way to reduce side effects without stopping the drug?
Sometimes. For methotrexate, taking folic acid daily reduces nausea and mouth sores. For steroids, taking them in the morning can help with sleep and reduce adrenal suppression. Switching to a different drug in the same class might help-like going from prednisone to a lower-dose inhaled steroid. Never change your dose without talking to your doctor, but ask about options. Many side effects are manageable with small adjustments.
What’s the most important thing I should know?
You are not alone, and you are not powerless. Millions live with immunosuppression and lead full lives. The key is knowledge, vigilance, and communication. Know your drug, know your risks, know your body’s signals, and never hesitate to speak up when something feels off. Your medical team is there to help you balance safety and health-not to scare you, but to empower you.


Ryan Tanner
October 31, 2025 AT 21:55Just wanted to say I’m on Humira and honestly? I’ve had zero serious infections. Yeah, I got shingles once-scary as hell-but I caught it early because I listen to my body. Wear the mask, wash your hands, don’t panic. You’re not broken, you’re just playing a harder game. And hey, you’re still out here living. 🙌
Jessica Adelle
November 2, 2025 AT 00:31It is an absolute disgrace that our healthcare system allows such dangerous pharmaceuticals to be prescribed with such minimal oversight. The FDA is complicit in this public health catastrophe. These drugs are not medicine-they are chemical surrender. I would rather die with dignity than be chemically neutered by Big Pharma’s profit-driven agenda.
Sai Ahmed
November 3, 2025 AT 13:39Did you know the CDC is hiding data on vaccine deaths in immunocompromised people? I’ve seen the internal memos. They don’t want you to know that biologics are linked to brain fog, chronic fatigue, and spontaneous organ failure. Your doctor won’t tell you this. They’re paid by the pharma giants. Just ask yourself: why do they keep pushing more drugs and not more natural healing?
Albert Schueller
November 5, 2025 AT 11:10Immunosuppresants are a joke. The fact that people are taking methotrexate and not even getting regular liver panels is criminal. I know a guy who died from PML because his doctor didn't check his JC virus status. And now we're supposed to trust these so-called 'experts'? The system is rigged. And don't even get me started on the flu shot-mRNA is just a Trojan horse for nano-chips.
Ted Carr
November 6, 2025 AT 09:39So let me get this straight: you’re telling me the same people who told us to ‘just wear a mask’ now want us to take drugs that make us more vulnerable to fungal brain infections? And we’re supposed to be grateful? Wow. Just… wow. I’m starting to think the real autoimmune disease is trust in authority.
Rebecca Parkos
November 7, 2025 AT 00:14THIS. RIGHT HERE. I’m a lupus warrior and I’ve been hospitalized three times because I waited too long. I’m screaming into the void here: IF YOU FEEL OFF, GO TO THE ER. NO EXCUSES. I lost my cousin because he thought ‘it’s probably just allergies.’ It was pneumocystis pneumonia. He was 34. Don’t be him. Call your doctor NOW. Don’t wait for a fever. Your body is screaming in a language you’ve been trained to ignore. LISTEN.
Bradley Mulliner
November 8, 2025 AT 03:22Anyone who takes these drugs is making a conscious choice to trade long-term health for short-term comfort. You think you’re controlling your disease? No. You’re surrendering to it. And now you want praise for being ‘brave’? You’re not brave-you’re irresponsible. If your body can’t handle the natural course of illness, maybe you shouldn’t be out in public at all. You’re a walking biohazard.
Rahul hossain
November 9, 2025 AT 03:20One must wonder, dear interweb wanderers, whether the modern age has replaced the soul’s resilience with the cold calculus of chemical control. We have traded the wisdom of ancestral healing for the glittering promises of patent-protected potions. Is it not poetic, in a tragic sense, that we now carry emergency cards not to declare our love, but to declare our vulnerability? The body, once a temple, is now a laboratory. And we, the faithful, kneel before the altar of the pill bottle, whispering: ‘Please, let me live another day.’