When someone vomits blood or passes black, tarry stools, it’s not just a bad stomach bug-it’s a medical emergency. Upper gastrointestinal (GI) bleeding can happen to anyone, but it’s most common in older adults and those with liver disease or long-term use of painkillers. Every year, about 100 out of every 100,000 adults in the U.S. experience this. The good news? With fast action, most people survive. The bad news? Delayed care can be deadly. This isn’t about vague symptoms. It’s about recognizing the signs, knowing what’s causing it, and acting before it’s too late.
What Exactly Is Upper GI Bleeding?
Upper GI bleeding means blood is coming from somewhere in the upper part of your digestive tract-your esophagus, stomach, or the first part of your small intestine (duodenum). It’s not the same as rectal bleeding from hemorrhoids or colon issues. This is bleeding that happens above the ligament of Treitz, a key anatomical landmark. The most common causes? Peptic ulcers, swollen veins in the esophagus (varices), and irritation from medications or alcohol.
Peptic ulcers alone cause 40% to 50% of all cases. These are open sores in the stomach or duodenum, often caused by Helicobacter pylori infection or long-term use of NSAIDs like ibuprofen or aspirin. Esophageal varices, which happen in people with advanced liver disease, account for 10% to 20% of cases. These veins become enlarged and fragile from high pressure in the liver’s blood vessels. When they burst, the bleeding can be massive and fast.
Other causes include erosive gastritis (stomach lining worn away), Mallory-Weiss tears (rips from violent vomiting), and even cancer. Surprisingly, antidepressants like SSRIs can double your risk of bleeding, according to a 2022 study of half a million patients. And if you have liver disease, you’re also at risk for portal hypertensive gastropathy-a condition where the stomach lining bleeds slowly over time.
How Do You Know It’s Happening?
The symptoms are hard to ignore, but people often dismiss them. Hematemesis-vomiting blood-is the most obvious sign. Fresh blood looks bright red. If it’s been sitting in the stomach a while, it turns dark brown or black, like coffee grounds. That’s called ‘coffee-ground emesis.’ It’s not just gross-it’s a red flag.
Melena is another key sign: black, sticky, foul-smelling stools. This happens when blood travels through the intestines and gets digested. It’s not the same as eating beets or taking iron pills. If your stool looks like tar and smells like it’s been sitting in the sun, get checked.
Signs of shock are more subtle but more dangerous. A fast heart rate (over 100 beats per minute), dizziness, cold skin, or fainting mean your body is losing blood and struggling to keep up. Low blood pressure (below 90 mmHg systolic) is a late sign. By then, you’ve already lost a lot. A study in the Annals of Internal Medicine found that a blood urea nitrogen (BUN) to creatinine ratio above 30:1 is 69% accurate at pointing to upper GI bleeding-even before imaging or endoscopy.
Don’t wait for all these symptoms. If you’ve vomited anything that looks like blood, or had black stools for more than a day, go to the ER. There’s no such thing as ‘maybe it’s nothing’ when it comes to GI bleeding.
Why Timing Is Everything
Speed saves lives. The Glasgow-Blatchford score is the tool doctors use to decide how urgently you need help. It’s not a guess-it’s based on hard numbers: your hemoglobin level, blood pressure, heart rate, whether you have melena, if you’ve fainted, and if you have liver or heart disease. A score of 2 or higher means you need hospital care. A score of 0? You might be safe to go home.
That’s a game-changer. Dr. Robert Logan from Harvard says this score now identifies 15% of patients who don’t need to be admitted at all. But here’s the problem: too many hospitals still wait too long to do the key test-endoscopy.
Current guidelines say endoscopy should happen within 24 hours. But the best outcomes come when it’s done within 12 hours. A 2022 study showed that doing endoscopy early cuts death rates by 25%. Hospitals that use a standardized ‘Upper GI Bleed Bundle’-with rapid assessment, risk scoring, and strict timing-have dropped their 30-day death rate from 8.7% to 5.3%.
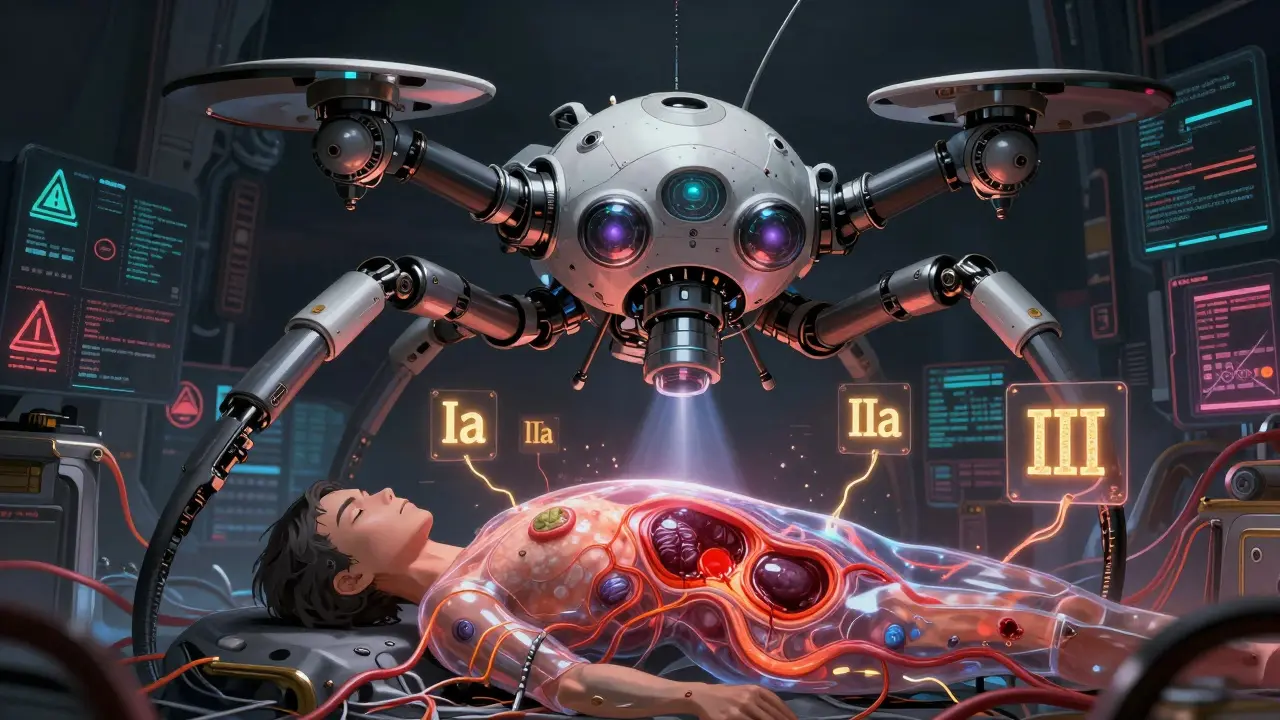
During endoscopy, doctors use the Forrest classification to judge how dangerous the bleeding is. Class Ia-blood spurting out-is the worst. Without treatment, 90% of these cases rebleed. Class IIa-visible blood vessel-is also high risk. Class III-no active bleeding-is low risk. This isn’t just for diagnosis. It tells the doctor exactly what treatment to use right then and there.
How Doctors Stop the Bleeding
There are two main types of upper GI bleeding: non-variceal (like ulcers) and variceal (like swollen veins). They’re treated very differently.
For ulcers and erosions, the first step is high-dose proton pump inhibitors (PPIs). You get an 80mg IV push, then a continuous drip of 8mg per hour. This isn’t just to reduce acid-it’s to help clots stay in place. The COBALT trial showed this cuts rebleeding from 22.6% down to 11.6%. Then comes endoscopic treatment: injecting epinephrine to narrow blood vessels, using heat or clips to seal the spot. Together, these stop bleeding in 90% to 95% of cases.
For varices, the approach is more urgent. You get terlipressin or octreotide right away-drugs that lower pressure in the liver’s veins. You also get antibiotics like ceftriaxone to prevent deadly infections. Then, band ligation. That’s when tiny rubber bands are placed around the varices to cut off blood flow. It’s far better than older methods like injecting chemicals. Banding cuts rebleeding from 60% to 25%.
Transfusions are needed if your hemoglobin drops below 7 g/dL or you’re dizzy and weak. But don’t overdo it. Giving too much blood can raise pressure in the liver and make varices worse. The goal is 7-9 g/dL. Each unit of packed red cells raises your hemoglobin by about 1 g/dL.
What Happens After the Bleeding Stops?
Stopping the bleeding is only half the battle. The other half is preventing it from coming back.
If you had an ulcer, you’ll need testing for Helicobacter pylori. If it’s positive, you’ll get a two-week course of two antibiotics and a PPI. If you take NSAIDs, you’ll need to stop them-or switch to something safer. If you’re on SSRIs, your doctor will weigh the risks and benefits. Many patients stop these meds on their own after a bleed, but that can lead to depression relapse. Talk to your doctor.
If you had varices, you’ll need long-term treatment. Beta-blockers like propranolol or nadolol are often prescribed to lower pressure in the veins. You’ll also need regular endoscopies every 1-2 years to check for new varices. In some cases, a shunt procedure (TIPS) is needed to reroute blood flow around the liver.
Follow-up matters. A 2022 study found that 68% of patients felt anxious about another bleed within 30 days. Many changed their diets-cutting out alcohol, spicy food, caffeine. Some quit NSAIDs without asking their doctor. That’s dangerous. You need a plan.

What’s New in 2025?
Technology is changing how we treat this. In 2023, the FDA approved Hemospray, a powder that sticks to bleeding spots like a bandage. It’s not a cure, but it’s a lifesaver when other methods fail. It worked in 92% of tough cases in a 2022 trial.
Even bigger? AI-assisted endoscopy. In 2023, a study showed AI systems spotted bleeding signs with 94.7% accuracy-way better than human eyes at 78.3%. These systems are being rolled out in major hospitals now. But there’s a catch: they were trained mostly on data from white patients. In Black and Hispanic patients, accuracy drops by 15%. That’s a serious gap.
The NIH is now running the UGIB-360 study, tracking 10,000 people to build personalized risk models using DNA, gut bacteria, and clinical history. Results are due by late 2025. That could mean future treatments aren’t one-size-fits-all-they’re tuned to your body.
What You Can Do
You can’t always prevent upper GI bleeding, but you can reduce your risk:
- Don’t take NSAIDs long-term without a PPI if you’re over 60 or have a history of ulcers.
- Limit alcohol-especially if you have liver disease.
- Get tested for Helicobacter pylori if you’ve had an ulcer before.
- Don’t ignore black stools or vomiting blood. Call your doctor or go to the ER.
- If you’re on SSRIs, talk to your doctor about your bleeding risk.
And if you’ve had a bleed before, make sure you have a follow-up plan. Don’t assume it’s over just because the bleeding stopped. The real work begins after you leave the hospital.
Can upper GI bleeding be fatal?
Yes, especially if treatment is delayed. Esophageal varices have a 20% death rate within six weeks without treatment. Even ulcers can be deadly if they cause massive blood loss or rebleed. Early endoscopy and proper management reduce mortality to under 6% in well-managed cases.
Is black stool always a sign of bleeding?
Not always. Iron supplements, bismuth (like Pepto-Bismol), or eating large amounts of dark foods like black licorice can cause dark stools. But if you haven’t taken these and your stool is black, sticky, and smells foul, it’s likely melena from GI bleeding. When in doubt, get it checked.
Can I treat upper GI bleeding at home?
No. Upper GI bleeding is a medical emergency. Even if you feel fine after vomiting blood, you could be losing blood internally. Home remedies like antacids or herbal teas won’t stop active bleeding. Delaying care increases the risk of death. Always seek emergency care.
How long does recovery take after a GI bleed?
Recovery varies. Most people stay in the hospital for 3-7 days. If you had an ulcer, you’ll need to take PPIs for 4-8 weeks. For varices, lifelong monitoring and medication are often needed. Full recovery can take weeks to months, depending on your age, other health conditions, and how much blood you lost.
Are there any new treatments on the horizon?
Yes. AI-powered endoscopy is already being used in major hospitals to catch subtle bleeding spots. Hemospray is a new tool for hard-to-control bleeding. And by late 2025, we’ll have data from the NIH’s UGIB-360 study, which aims to predict individual risk using genetics and gut bacteria-leading to truly personalized care.
Paul Ong
January 1, 2026 AT 02:03Vomiting blood is not something you shrug off
Go to the ER. Period.
Richard Thomas
January 2, 2026 AT 20:38It's fascinating how medicine has shifted from reactive to predictive in upper GI bleeding. The Glasgow-Blatchford score isn't just a tool-it's a philosophical shift in how we define urgency. We used to treat symptoms, now we treat risk profiles. And yet, the human element remains irreplaceable. A patient's fear, their hesitation, their refusal to believe it's serious-that's often the real bottleneck. Technology gives us precision, but empathy gives us compliance. The AI endoscopy systems are impressive, sure, but they don't sit with a patient who's terrified after their third black stool. They don't hear the quiet voice saying 'I didn't want to be a burden.' That's the part no algorithm can quantify.
Ann Romine
January 4, 2026 AT 13:12I'm from a rural community where people still wait days before going to the ER. My aunt ignored melena for a week because she didn't have transportation. She ended up in ICU. This post should be printed and posted in every pharmacy and gas station in the Midwest. We need outreach, not just data.
Todd Nickel
January 6, 2026 AT 10:07The BUN:Cr ratio >30 being 69% accurate is clinically significant but underutilized. Most EDs still rely on vague clinical gestalt until endoscopy. There's a gap between evidence and practice. Also, the Hemospray data is promising but the cost-benefit analysis hasn't been fully explored in community hospitals. And the AI bias issue-15% drop in accuracy for non-white patients-isn't just a technical flaw, it's an ethical failure. Training data must be demographically representative, or we're building a system that kills people of color at higher rates. This isn't sci-fi-it's happening now.
Austin Mac-Anabraba
January 6, 2026 AT 20:47Let's be honest-the real cause of this epidemic is Big Pharma pushing NSAIDs like candy and the medical establishment rewarding profit over prevention. SSRIs? They're chemical lobotomies disguised as treatment. The system doesn't want you healthy. It wants you medicated, monitored, and returning every month. They'll give you a $20,000 endoscopy but won't give you a $50 vitamin D test. The bleeding is just a symptom of a broken healthcare machine.
Phoebe McKenzie
January 8, 2026 AT 05:22I've seen this too many times. People think they can 'tough it out' like it's some kind of manly test. You don't 'wait and see' when your insides are pouring out. This isn't a suggestion-it's a death sentence if ignored. And don't even get me started on doctors who don't do endoscopy within 12 hours. They're playing Russian roulette with your life. Someone should sue these hospitals for negligence.
gerard najera
January 9, 2026 AT 09:58Coffee-ground emesis = bleed. Black stool = bleed. Don't overthink it.
Stephen Gikuma
January 9, 2026 AT 15:04Who funds these 'studies'? The same corporations that make PPIs and endoscopy gear. The real solution? Stop eating processed food. Stop drinking chemical-laced soda. Stop taking pills that make you dependent. The body heals itself if you stop poisoning it. They don't want you to know that because it doesn't make money. The FDA approved Hemospray? More like a cash grab. Real medicine is food, rest, and clean water-not high-tech band-aids.
Layla Anna
January 11, 2026 AT 10:54I had a friend who ignored black stools for 3 days... she thought it was just her iron pills. By the time she went in, she needed 5 units of blood and a stint in the ICU. I cried for a week. Please, if you're reading this and you're even a little worried-go. Just go. I'm so glad she's okay now but it scared me for life 😭
Heather Josey
January 12, 2026 AT 21:42This is one of the most comprehensive and clinically accurate summaries I've seen on this topic. The emphasis on early endoscopy within 12 hours is critical-many institutions still operate on outdated protocols. The data on PPI dosing and band ligation efficacy is spot-on. I've shared this with my entire medical team. We're updating our internal guidelines next week. Thank you for the clarity and evidence-based approach. This is the kind of content that saves lives.
Donna Peplinskie
January 13, 2026 AT 02:59I'm from Canada, and we've had similar challenges with rural access to timely endoscopy. But we've implemented regional GI bleed hubs-where patients are rapidly transferred to centers with 24/7 endoscopy teams. It reduced mortality by 30% in our province. The key? Coordinated care, not just tech. Also, I love that you mentioned the UGIB-360 study. Personalized medicine is the future. I hope they include gut microbiome data from Indigenous populations too-there's so much we haven't explored.
Andy Heinlein
January 14, 2026 AT 02:14Just had my first GI bleed last year. Turns out it was from years of ibuprofen for back pain. I thought it was just 'stomach issues'. I'm on PPI now, stopped the NSAIDs, and actually feel better than I have in years. Also, I stopped drinking. Who knew? Life's weird like that. Anyway, if you're reading this and you're on painkillers daily-talk to your doc. Don't wait until you're puking coffee grounds 😅
Bobby Collins
January 15, 2026 AT 18:20AI endoscopy? Yeah right. I heard the government is putting microchips in the cameras to track you. They already know if you've been to the ER. They're using this bleeding thing to push vaccines and biometric IDs. Don't trust the hospitals. They're all connected. I'm not going near one until the truth comes out.