Combining alcohol with prescription drugs isn’t just a bad idea-it can be deadly. Many people think having one drink with their meds is harmless, especially if they’ve done it before without issues. But the science says otherwise. Every year, thousands of people end up in emergency rooms because they didn’t realize how dangerous mixing alcohol with their medications can be. In 2022 alone, alcohol and prescription drug interactions were linked to over 2,300 overdose deaths in the U.S., according to CDC data. And it’s not just heavy drinkers at risk. Even one drink can tip the balance when paired with certain pills.
How Alcohol Changes How Your Medicines Work
Alcohol doesn’t just sit there while your medicine does its job. It actively interferes with how your body processes drugs. There are two main ways this happens: pharmacokinetic and pharmacodynamic interactions.
Pharmacokinetic interactions affect how your body absorbs, breaks down, or eliminates the drug. Most medications are processed in the liver by enzymes called cytochrome P450. Alcohol messes with these enzymes. If you drink regularly, your body starts making more of a specific enzyme-CYP2E1-to break down alcohol faster. That means drugs like propranolol (used for high blood pressure) get cleared out too quickly, making them less effective. Studies show this can reduce their effectiveness by 30% to 50%.
On the flip side, if you drink just once or occasionally, alcohol can block those same enzymes. This causes drugs like warfarin (a blood thinner) to build up in your blood. One study found alcohol can increase warfarin levels by up to 35%, raising your risk of dangerous bleeding. This isn’t theoretical-it’s happened to real people who thought a glass of wine with their pill was fine.
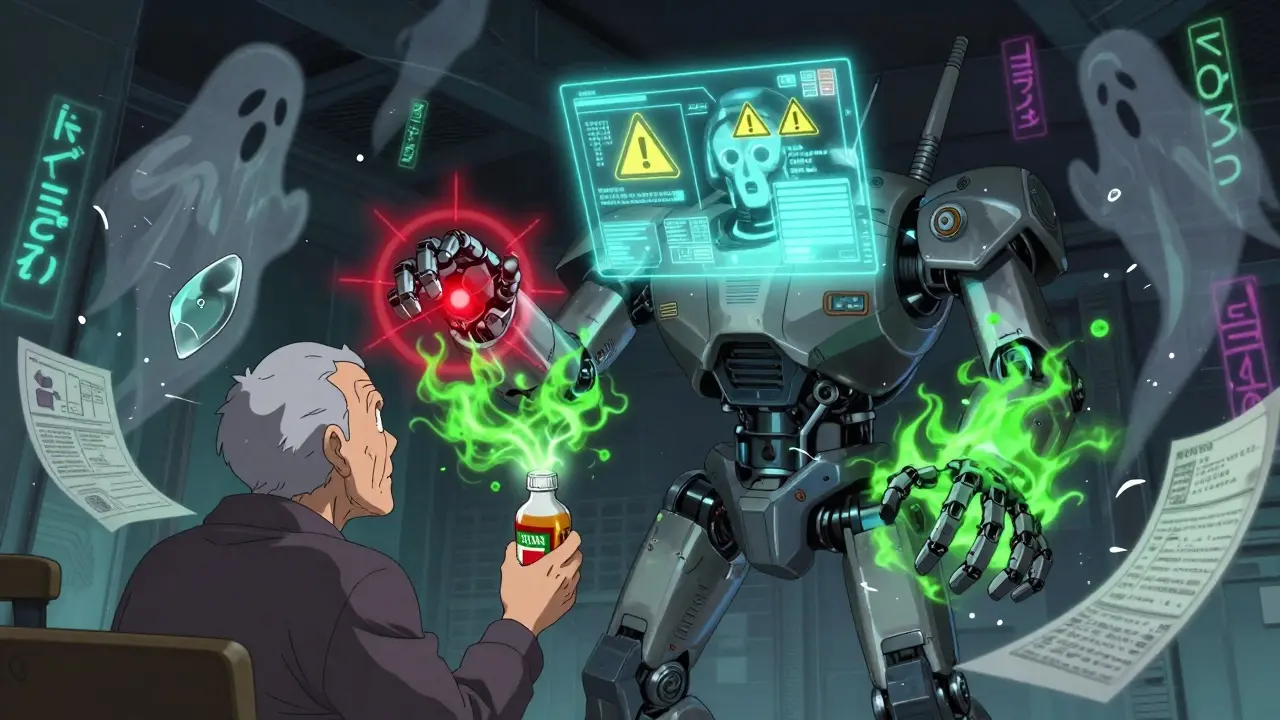
Pharmacodynamic interactions are even more dangerous. These happen when alcohol and a drug amplify each other’s effects on your body. This is especially true for central nervous system depressants. Think of it like stacking two heavy weights on a scale-you don’t just add weight, you overload the system.
The Deadliest Combinations
Some medications are absolutely not safe with alcohol. The highest-risk group includes opioids and benzodiazepines.
Opioids like oxycodone, hydrocodone, and fentanyl already slow your breathing. Alcohol does the same. Together, they multiply the risk of respiratory failure by six times. The CDC reports that alcohol-opioid combinations account for 26% of all prescription drug overdose deaths. And you don’t need to be drunk for this to happen. A blood alcohol level as low as 0.02%-the equivalent of one standard drink-can double the risk of a fatal crash when combined with therapeutic opioid doses.
Benzodiazepines like diazepam (Valium), alprazolam (Xanax), and lorazepam (Ativan) are prescribed for anxiety, insomnia, or seizures. Alcohol turns these drugs into a sedative bomb. Research shows the combination increases sedation by 400% compared to either substance alone. In older adults, this leads to a 50% higher chance of falling. Falls are the leading cause of injury-related death in people over 65. One study found that 78% of falls in nursing homes involving sedatives happened in patients who drank alcohol within six hours.
Even antidepressants aren’t safe. SSRIs like sertraline or fluoxetine might seem harmless with a drink, but they can make you drowsy, dizzy, or uncoordinated. A clinical review found that 35% of patients over 65 experienced clinically significant drowsiness after just one or two drinks with their SSRI. That’s enough to make walking risky, especially on slippery floors or stairs.
Other Dangerous Pairings
It’s not just the big-name drugs. Some common medications carry hidden risks.
NSAIDs like ibuprofen and naproxen are often taken for pain or inflammation. Mix them with alcohol, especially if you drink heavily (three or more drinks a day), and your risk of stomach bleeding skyrockets by 300%. That’s not a typo. One study tracking 200,000 patients showed that heavy drinkers on NSAIDs were three times more likely to bleed internally than those who avoided alcohol.
Acetaminophen (Tylenol) is another silent killer. It’s in hundreds of over-the-counter cold and pain medicines. Your liver normally breaks it down safely. But when alcohol is in the system, it creates a toxic byproduct called NAPQI. In regular drinkers, this can cause acute liver failure. The FDA estimates that 1 in 200 people who regularly drink alcohol and take acetaminophen will develop serious liver damage. Many don’t even realize they’re taking acetaminophen-because it’s hidden in combination pills like Vicodin or Excedrin.
Even some antibiotics can be risky. Isoniazid, used for tuberculosis, can cause severe liver damage when mixed with alcohol. About 15% of users experience toxic reactions. Other antibiotics like metronidazole can cause nausea, vomiting, and rapid heartbeat when combined with alcohol-even a single sip.
Who’s Most at Risk?
Not everyone faces the same level of danger. Certain factors make interactions worse.
Age is a major one. People over 65 metabolize alcohol and drugs more slowly. Their livers don’t work as well, and they have less water in their bodies, meaning alcohol stays concentrated longer. Studies show older adults experience 3.2 times more severe interactions than younger people.
Gender matters too. Women generally have less body water and more body fat than men. That means alcohol hits their bloodstream harder and stays longer. Women face about 20% higher interaction severity for the same amount of alcohol.
Pre-existing liver disease is another red flag. If your liver is already damaged from hepatitis, fatty liver, or past alcohol use, even small amounts of alcohol can trigger severe reactions with medications like acetaminophen. Risk increases fivefold in these patients.
And then there’s the problem of unawareness. A 2023 WebMD survey found that 57% of adults believe one drink is safe with most medications. Thirty-two percent think only hard liquor causes problems-ignoring that beer and wine are just as dangerous. Many patients say their doctors never warned them. Healthgrades data shows 68% of people prescribed benzodiazepines were never told to avoid alcohol.
What Should You Do?
If you take prescription medication, don’t guess. Here’s what to do instead:
- Check the label. Look for warnings like "Do not drink alcohol" or "May cause drowsiness." But don’t rely on this alone-only 38% of benzodiazepine prescriptions even include alcohol warnings.
- Talk to your pharmacist. Pharmacists are trained to catch these interactions. Use the four-question screening tool they’re taught: "Do you drink alcohol? How often? How much? Have you noticed any side effects?" This method has 92% accuracy in identifying risky combinations.
- Use a reliable app. The NIAAA’s "Alcohol Medication Check" app lets you scan your prescription barcode and instantly see if alcohol is risky with that drug. It covers over 2,300 medications.
- Ask your doctor directly. Say: "Is it safe to have even one drink with this medication?" Don’t let them brush you off. If they don’t know, ask for a pharmacist consult.
Some doctors argue that for low-risk meds, a single drink might be okay under supervision. But experts from the American Geriatrics Society, CDC, and NIAAA all agree: when in doubt, skip it. The consequences aren’t worth the risk.

What’s Changing in Healthcare?
The system is slowly waking up. In 2022, the U.S. passed the Alcohol-Drug Interaction Labeling Act, requiring explicit "ALCOHOL WARNING" labels on high-risk prescriptions. That affects over 147 million prescriptions a year.
Hospitals are using real-time clinical systems that flag interactions before a drug is even dispensed. Facilities with full implementation have seen a 28% drop in alcohol-related adverse events. The VA system mandates alcohol screening for all patients on medications-89% of VA hospitals do it. Only 32% of private practices do.
And now, AI is stepping in. Epic Systems rolled out a machine learning tool in 2024 that analyzes over 200 patient variables-age, weight, liver function, drinking habits-to predict individual interaction risk. It’s 89% accurate, according to a study in NEJM Evidence.
But technology won’t fix the biggest problem: people don’t listen. A 2023 study found only 28% of high-risk patients stop drinking completely, even after being warned. Many think they’re fine because they’ve "always done it this way." But medicine doesn’t work on luck. It works on science.
Bottom Line
There’s no safe amount of alcohol with many prescription drugs. The risks aren’t just theoretical-they’re documented, measured, and deadly. Whether it’s your blood pressure pill, your anxiety med, or your painkiller, alcohol can turn a routine treatment into a life-threatening event.
If you’re unsure, don’t take the chance. Talk to your pharmacist. Use the NIAAA app. Ask your doctor again. Your body doesn’t have a second chance to recover from liver failure, respiratory arrest, or a fatal fall. One drink might seem harmless. But when it’s mixed with a prescription drug, it’s not just a drink-it’s a gamble with your life.
Can I have one drink with my prescription medication?
It depends on the medication. With opioids, benzodiazepines, or sleep aids, even one drink can be dangerous. With some antibiotics or blood pressure drugs, it might be low risk-but only if you’re healthy and don’t drink often. The safest answer is always: check with your pharmacist or doctor. Don’t assume it’s okay just because you’ve done it before.
What should I do if I accidentally mixed alcohol with my meds?
If you feel dizzy, confused, extremely sleepy, or have trouble breathing, seek emergency help immediately. Call 999 or go to the nearest A&E. Don’t wait. These symptoms can escalate quickly, especially with opioids or benzodiazepines. If you’re not having symptoms, call your pharmacist or doctor anyway. They can advise you on what to watch for over the next few hours.
Do over-the-counter meds interact with alcohol too?
Yes. Many OTC drugs contain acetaminophen, NSAIDs, or antihistamines-all of which can react badly with alcohol. Cold and flu medicines often have hidden acetaminophen. Pain relievers like ibuprofen increase stomach bleeding risk. Sleep aids like diphenhydramine (Benadryl) can make you dangerously drowsy when mixed with alcohol. Always read the label and look for "alcohol warning" or "do not consume with alcohol."
Why don’t doctors always warn patients about alcohol interactions?
Time constraints, assumption that patients already know, or lack of training. A 2023 study found 43% of primary care doctors couldn’t correctly identify all high-risk medication classes. Many assume patients will read the label, but only 65% of high-risk prescriptions even include alcohol warnings. It’s a system failure, not a patient failure. That’s why you need to ask-don’t wait to be told.
Are there any medications that are safe with alcohol?
Some antibiotics like amoxicillin or penicillin have minimal interaction risk. Certain cholesterol meds like atorvastatin are generally safe in moderation. But "safe" doesn’t mean "risk-free." Even these can cause drowsiness or stomach upset when mixed with alcohol. The safest approach is to avoid alcohol entirely while on any new medication until you’ve confirmed it’s okay with your pharmacist.
Can I drink alcohol the day before or after taking my meds?
It depends on the drug’s half-life. Some medications stay in your system for days. For example, fluoxetine (Prozac) can linger for up to two weeks. Alcohol consumed the day before can still interact. If you’re on a long-acting drug like extended-release oxycodone or daily warfarin, avoid alcohol for at least 24 hours before and after. When in doubt, wait 48 hours. Your liver needs time to clear both substances.


Kegan Powell
January 27, 2026 AT 14:18Man, I never realized how sneaky this stuff is. I thought one glass of wine with my blood pressure med was fine 'cause I've done it for years. Turns out my liver's been doing backflips the whole time 😅
April Williams
January 28, 2026 AT 06:14People are so careless. You think you're being smart by having one drink but you're just one bad combo away from an autopsy. Stop being lazy and read the damn label. This isn't rocket science, it's basic survival.
Harry Henderson
January 28, 2026 AT 07:42If you're still drinking while on meds, you're not just risking your life-you're disrespecting every doctor, pharmacist, and scientist who spent decades studying this. Wake up. Your hangover isn't worth a hospital stay.
suhail ahmed
January 29, 2026 AT 01:31In India, we call this 'jugaad'-fixing things with duct tape and hope. But when it comes to your body? No jugaad. One drink with warfarin? That’s not a toast, that’s a suicide note written in ethanol. Stay safe, brothers and sisters.
Candice Hartley
January 29, 2026 AT 17:40I had no idea Tylenol + alcohol could wreck your liver. I’ve been taking it for migraines and having a beer after. 😳 I’m calling my pharmacist tomorrow.
astrid cook
January 30, 2026 AT 13:53Honestly? People who mix alcohol and meds are just selfish. They don’t care about the cost to the healthcare system, the ER nurses, or their family when they’re in a coma. This isn’t a personal choice-it’s a public health failure.
Andrew Clausen
February 1, 2026 AT 06:43The article claims 'one drink' can be deadly, but fails to define 'one drink.' Is it 12 oz of beer? 5 oz of wine? 1.5 oz of whiskey? Precision matters. Also, 'over 2,300 overdose deaths' doesn't specify if alcohol was the primary cause or a contributing factor. Correlation ≠ causation.
Anjula Jyala
February 1, 2026 AT 11:32CYP2E1 induction is a well-documented phenomenon in pharmacokinetics. Chronic ethanol exposure upregulates phase I metabolism, leading to subtherapeutic concentrations of CYP3A4 and CYP2D6 substrates. Concurrent inhibition via acute intake causes toxic accumulation. The data is robust. Stop anecdotalizing.
Kirstin Santiago
February 2, 2026 AT 14:33I work in a nursing home. Saw a woman fall after her Valium and a glass of wine. Broke her hip. She cried saying she didn't know it was a problem. We need better education-not just labels. Maybe a quick video at the pharmacy counter? Just a thought.
Kathy McDaniel
February 3, 2026 AT 09:54ok so i just read this and i think i might’ve been dumb. i take sertraline and sometimes have a glass of wine to unwind. i’ve never felt weird but now im scared. gonna ask my doc tmrw. thanks for the wake up call 🙏