What a DEXA Scan Actually Measures
A DEXA scan isn’t just another X-ray. It’s the most trusted way to measure bone mineral density - how much calcium and other minerals are packed into your bones. The machine uses two very low-dose X-ray beams, one high-energy and one low-energy, to tell the difference between bone and soft tissue. It’s quick, painless, and exposes you to less radiation than a day spent outside in the sun. Most scans focus on your lower spine and hip, because those are the spots most likely to break if your bones get weak.
The result? A number - your T-score. This tells you how your bone density compares to that of a healthy 30-year-old adult of the same sex. It’s not a diagnosis on its own, but it’s the starting point for figuring out your risk. A T-score of -1.0 or higher means your bones are normal. Between -1.0 and -2.5? You have osteopenia - low bone mass. At -2.5 or lower? That’s osteoporosis. These numbers aren’t guesses. They’re backed by decades of research and used by doctors worldwide to make real treatment decisions.
Why T-Scores Matter More Than You Think
Many people walk out of their DEXA scan with a printout full of numbers and no idea what they mean. The T-score is the key. But here’s the catch: it doesn’t tell you everything. A T-score of -2.7 might sound scary, but if you’ve never broken a bone, are active, and don’t smoke, your actual fracture risk might be lower than someone with a -2.0 score who’s had two hip fractures already. That’s why doctors don’t just look at the number. They look at your life.
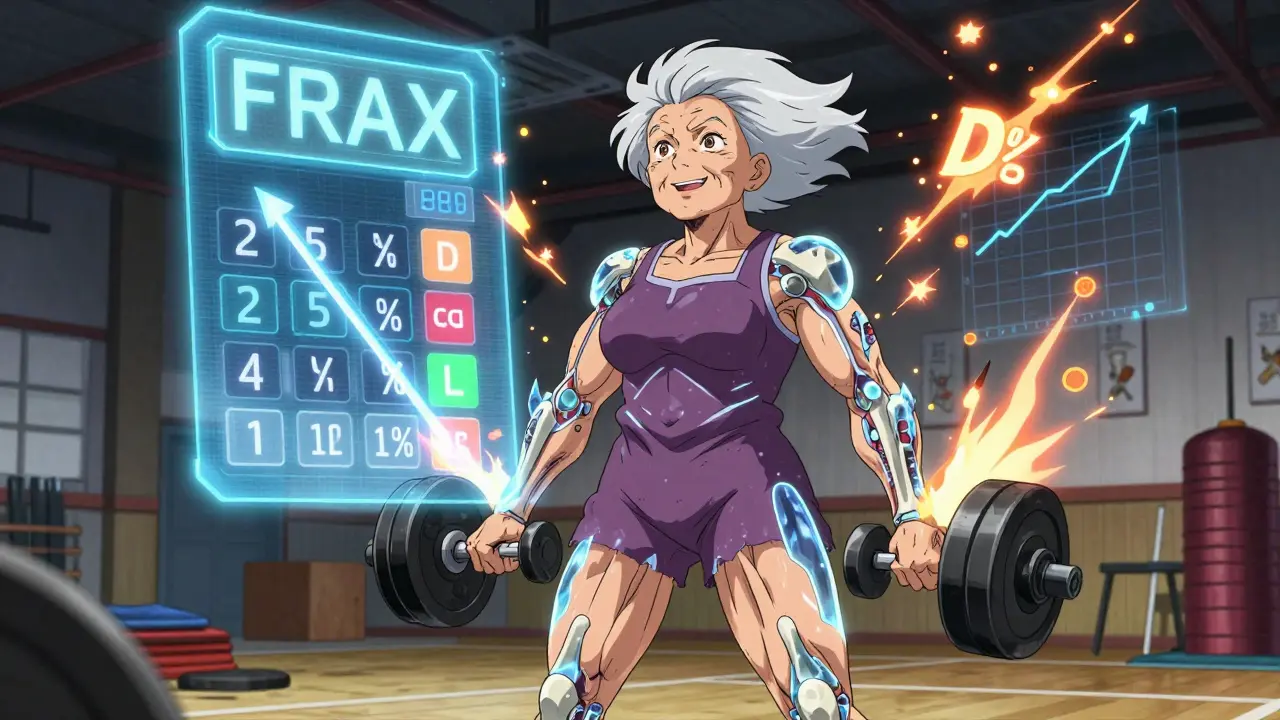
The FRAX tool is what they use to put it all together. It takes your T-score and adds in your age, weight, whether you’ve had a previous fracture, if you smoke, if you drink alcohol, if you take steroids, and even your family history. It then calculates your chance of breaking a bone in the next 10 years. That’s the number that decides whether you need medication or just lifestyle changes. One study showed FRAX improves accuracy by up to 22% compared to using DEXA alone. If your doctor skips FRAX, ask why.
Who Really Needs a DEXA Scan?
You don’t need a DEXA scan just because you’re over 50. Medicare and most insurers cover it for specific groups. In the UK, the NHS recommends screening for women over 65 and men over 70. But if you’re younger and have risk factors, you might need it sooner. These include: a parent who broke a hip, long-term steroid use (like prednisone), early menopause before 45, rheumatoid arthritis, or a height loss of more than 1.5 inches. If you’ve broken a bone from a minor fall - like dropping from a standing height - that’s a red flag, no matter your age.
Here’s the reality: about 40% of women over 50 will break a bone because of weak bones. But only about half of them ever get tested. That’s not because they’re not at risk - it’s because they don’t know they should be screened. If you’re in one of these higher-risk groups and haven’t had a scan, talk to your GP. It’s a simple 10-minute test that could prevent a life-changing injury.
What DEXA Can’t Tell You
DEXA is great - but it’s not perfect. It can’t tell if your bones are brittle inside, only how dense they are. Two people with the same T-score can have very different bone structures. That’s why some newer tools are being added. One is the Trabecular Bone Score (TBS), which looks at the texture of your spine on the DEXA image. A rougher texture means weaker internal structure, even if the density looks okay. Studies show TBS improves fracture prediction by 12-18%.
Another limitation? DEXA can be thrown off by arthritis, metal implants, or calcium deposits in your arteries. If you’ve had spinal fusion or severe degenerative disease, your spine scan might not be reliable. In those cases, your doctor might focus on your hip instead. And if you’re very thin or very muscular, the results can be harder to interpret. That’s why it’s so important to have the scan done by a certified technician - someone trained to spot these issues before they mess up your results.
How Often Should You Get Scanned?
Most people don’t need to get a DEXA scan every year. If your first scan shows normal bone density, you might not need another for 10-15 years. If you have osteopenia and no other risks, repeat testing every 3-5 years is typical. If you’ve been diagnosed with osteoporosis and are on medication, you’ll usually get a scan every 1-2 years to see if treatment is working. But here’s the thing: if your numbers don’t change much over time, that’s actually good news. Bone density doesn’t bounce around like blood sugar. It moves slowly. Frequent scans won’t give you better info - they’ll just cost you more and expose you to more radiation, even if it’s tiny.
Insurance in the UK and US typically covers a scan every two years for those who qualify. If your doctor wants to do it more often, ask if it’s really necessary. Don’t let fear drive unnecessary tests.
What Happens After Your Results?
Getting a diagnosis of osteopenia or osteoporosis doesn’t mean you’re doomed. It means you have a chance to act. For mild cases, lifestyle changes can make a huge difference. Weight-bearing exercise - walking, dancing, lifting weights - is one of the best things you can do. So is getting enough vitamin D and calcium. Most adults need 800 IU of vitamin D daily, and 700-1200 mg of calcium from food or supplements. Quitting smoking and cutting back on alcohol also help.
If your fracture risk is high - say, over 20% in 10 years - your doctor may recommend medication. Bisphosphonates like alendronate or risedronate are common first-line options. They’re taken as pills once a week or monthly, and they’ve been shown to reduce spine fractures by up to 70% and hip fractures by about 40%. There are also injectable options like denosumab, which works every six months. These aren’t magic bullets, but they’re proven to work. And if you’re worried about side effects, talk to your doctor. Most people tolerate them well.
Real Stories, Real Outcomes
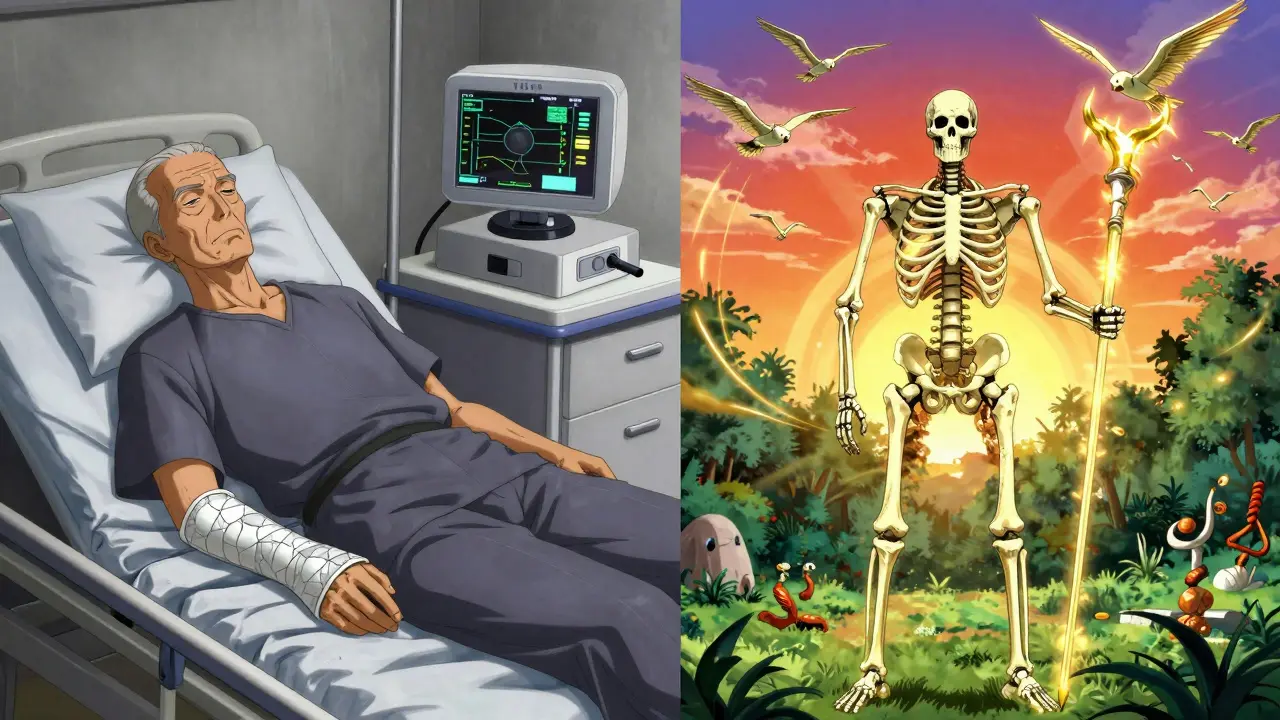
One woman in Bristol, 71, had no symptoms. She was active, walked every day, ate well. Her DEXA scan showed a T-score of -2.8. She was told she had osteoporosis. She started on medication, increased her vitamin D, and added strength training. Two years later, her repeat scan showed improvement. She didn’t just stop her bones from getting worse - they got stronger. She’s still walking, gardening, and traveling. That’s what this is about.
Another man, 68, broke his wrist after tripping on his rug. He thought it was just an accident. His GP ordered a DEXA scan. His T-score was -3.1. He’d had silent bone loss for years. Without that scan, the next fall could have broken his hip - and changed his life forever. He’s now on treatment and uses a cane on icy days. He says the scan saved him from a hospital stay.
Common Misconceptions
Many people think DEXA scans are dangerous because they use radiation. But one scan equals less than two days of natural background radiation. You get more from a cross-country flight. Others think osteoporosis only affects older women. It doesn’t. Men get it too. And while it’s more common in white and Asian populations, it affects all ethnic groups - and screening rates are lower in Black and Hispanic communities, which puts them at greater risk.
Another myth: if you feel fine, your bones are fine. Osteoporosis is called the silent disease for a reason. You don’t feel your bones thinning. The first sign is often a fracture. That’s why screening matters - even if you feel great.
What to Ask Your Doctor
- What’s my T-score and what does it mean for my fracture risk?
- Have you used FRAX to calculate my 10-year risk?
- Do I need medication, or can I manage this with diet and exercise?
- Should I get a Trabecular Bone Score (TBS) with this scan?
- How often should I repeat this test?
- Are there any conditions I have that could affect the accuracy of this scan?
If your doctor can’t answer these clearly, consider seeing a specialist - like an endocrinologist or a rheumatologist with experience in bone health. You deserve clear answers.
Final Thoughts
Bone health isn’t about being old. It’s about being informed. A DEXA scan is a simple, safe, and powerful tool that can catch problems before they turn into fractures. It doesn’t just give you a number - it gives you a chance. A chance to strengthen your bones, prevent pain, and keep living the life you love. Don’t wait for a fall to realize your bones need attention. Ask for the scan. Know your score. Take action.
What is a normal DEXA scan T-score?
A normal T-score is -1.0 or higher. This means your bone density is within one standard deviation of a healthy young adult. Scores between -1.0 and -2.5 indicate osteopenia (low bone mass), and -2.5 or lower means osteoporosis. These thresholds are set by the World Health Organization and used globally.
Is a DEXA scan painful or dangerous?
No, it’s not painful. You lie still on a table while the machine passes over you - it feels like a regular X-ray. The radiation dose is extremely low - less than you get from natural background sources in two days. For comparison, a chest X-ray is about 10 times higher. It’s considered very safe for most people.
Can I get a DEXA scan if I have metal implants?
Yes, but it may affect accuracy. Metal implants in the spine or hip can block the X-ray beam and cause falsely high readings. If you’ve had spinal fusion, hip replacement, or have significant arthritis, your doctor will likely focus on your hip or forearm instead. Always tell the technician about any implants before the scan.
How long does a DEXA scan take?
A full-body DEXA scan - spine and hip - typically takes about 10 to 15 minutes. You don’t need to fast or prepare specially. Wear loose clothing without metal zippers or buttons. You’ll be asked to lie still, but you won’t feel anything during the scan.
Does insurance cover DEXA scans in the UK?
Yes, the NHS covers DEXA scans for people who meet clinical risk criteria - including women over 65, men over 70, and younger individuals with risk factors like long-term steroid use, early menopause, or a history of fractures. Private scans are also available, typically costing between £80 and £150, depending on location.
Can exercise really improve bone density?
Yes - especially weight-bearing and resistance exercises. Walking, dancing, stair climbing, lifting weights, and using resistance bands stimulate bone growth. Studies show consistent exercise can slow bone loss and even improve T-scores slightly over time. It’s not a replacement for medication in high-risk cases, but it’s a powerful tool for everyone.
Why is my Z-score different from my T-score?
Your T-score compares you to a healthy 30-year-old - it’s used to diagnose osteoporosis. Your Z-score compares you to people your own age and sex. A low Z-score (below -2.0) in a younger person may signal an underlying condition causing bone loss, like thyroid disease or celiac disease. Doctors use Z-scores to look for secondary causes of low bone density.
What is Trabecular Bone Score (TBS) and should I ask for it?
TBS is an add-on analysis that looks at the texture of your spine on the DEXA image. It tells you about the internal structure of your bone - whether it’s strong and connected or thin and fragile. Studies show TBS improves fracture prediction by 12-18% beyond T-score alone. If you’re borderline or have osteopenia, asking for TBS can give you a clearer picture of your real risk.