Getting patients to take their meds as prescribed isn’t just about reminders or pill organizers. It’s about medication adherence-and that starts with goals that actually work. Too many treatment plans fail because they’re too vague: "Take your blood pressure pill every day." That’s not a goal. It’s a wish. The difference between someone sticking with their meds and someone skipping doses often comes down to one thing: how well the goal was built.
Why Most Adherence Efforts Fail
Patients aren’t lazy. They’re overwhelmed. A 2023 study found that 43% of people on chronic meds miss doses because they don’t understand why the pill matters, not because they forgot. Others struggle with cost, side effects, or just plain confusion. Self-reported adherence is wildly inaccurate-people think they’re taking 90% of their pills, but electronic tracking shows it’s more like 60%. That’s a huge gap. And if your doctor doesn’t know the real numbers, they can’t help.
Traditional methods-paper logs, phone calls, refill reminders-don’t cut it anymore. They’re reactive, not proactive. You’re waiting for someone to miss a dose before you notice. What works better? Goals that are clear, measurable, and tied to the patient’s life, not just their diagnosis.
The SMART Framework: Built for Real Life
The SMART goal model isn’t new, but it’s been perfected for healthcare. It stands for Specific, Measurable, Achievable, Relevant, and Time-bound. Here’s how to make it work for medication adherence:
- Specific: Instead of "Take your medicine," say: "Take my metformin 500mg with breakfast every morning at home." Who? Me. What? Metformin. Where? At home. When? With breakfast. Why? To control my blood sugar.
- Measurable: How will you know if you did it? Use pill counts, smartphone apps that log doses, or smart pill bottles that record openings. Even a simple checklist on the fridge counts.
- Achievable: Can the patient realistically do this? If they work two jobs and never eat breakfast, setting a goal to take pills with breakfast won’t stick. Adjust the time. Maybe it’s with their first cup of coffee after work.
- Relevant: Why does this matter to them? Not because the doctor said so. Because they want to stop feeling dizzy. Because they want to play with their grandkids without getting winded. Tie the goal to their personal why.
- Time-bound: Set a deadline. Not "start taking it better," but "I’ll take all my doses correctly for the next 14 days." Then review. Adjust. Celebrate.
A 2021 study from ThoroughCare showed patients who set SMART goals for their meds had a 65.5% adherence rate at follow-up-nearly double the average. The key? They didn’t just get a goal. They helped build it.
Don’t Skip the Barriers
There’s a smarter version of SMART called B-SMART. The "B" stands for Barriers. Before you even set the goal, ask: What’s standing in the way?
- Cost? Maybe switch to a generic or apply for patient assistance.
- Side effects? Talk to the provider-maybe the dose can be adjusted or the timing changed.
- Forgetfulness? Use a pill box with alarms or link doses to daily habits (brushing teeth, eating lunch).
- Health literacy? Don’t assume they understand "hypertension." Say "high blood pressure that can cause strokes."
- Transportation? If they can’t get to the pharmacy, ask about mail-order or delivery services.
One diabetes patient in a 2023 case study couldn’t take her insulin because she had to walk 45 minutes to the pharmacy. The solution? A free delivery program through her health plan. Her adherence jumped from 41% to 89% in six weeks. The goal didn’t change. The barrier did.
How to Track Progress-Without Overwhelming Anyone
Tracking doesn’t mean logging every dose in an app for 90 days. Start small. Here are three proven methods:
- Smart pill bottles: Devices like AdhereTech or Hero track when the bottle is opened. Accuracy? 98%. No patient input needed. Data syncs to a dashboard your provider can see.
- Pharmacy refill records: If someone hasn’t refilled their blood pressure med in 60 days, that’s a red flag. Medication Possession Ratio (MPR) is a reliable, low-tech way to spot trouble.
- Simple check-ins: A weekly text: "Did you take your pills yesterday? Yes/No." One-word answers. No pressure. Just data. A 2023 study found this increased adherence by 41% compared to no tracking.
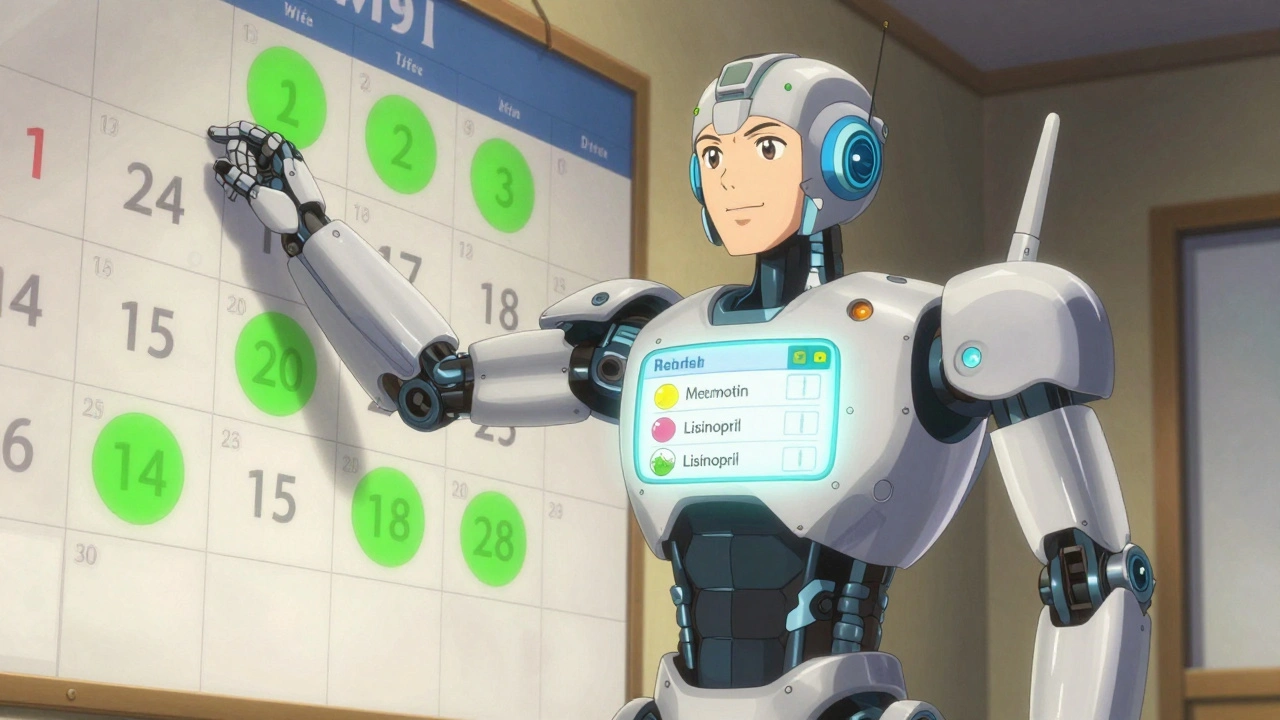
For patients who like visuals, color-coded calendars work wonders. A green sticker for each day they took their meds. A red one for missed. After a week, they can see their streak. That’s motivating. A 2023 survey found 78% of patients preferred this over digital graphs.
What Works Best for Different Conditions
Not all meds are the same. Goals should match the disease.
- Diabetes: Track fasting glucose levels alongside pill intake. A goal like "Take my metformin every morning and check my blood sugar twice a week for 30 days" links behavior to outcome.
- Hypertension: Use home blood pressure monitors. A goal: "Take my lisinopril every night and record my BP three times a week for 28 days."
- Asthma: Use smart inhalers like Propeller Health. They record when and where you use your inhaler. A goal: "Use my rescue inhaler no more than 2 times a week for the next month."
- Depression/Anxiety: Track mood alongside pill intake. "Take my sertraline every morning and rate my mood from 1-5 each night for two weeks."
Studies show that when goals connect meds to real outcomes-like fewer dizzy spells or more energy-adherence spikes. People don’t care about HbA1c numbers. They care about walking to the mailbox without stopping.
Common Pitfalls and How to Avoid Them
Even with SMART goals, things go wrong. Here’s what to watch for:
- Too many goals at once: Don’t ask someone to track pills, diet, exercise, and blood pressure all at once. Start with one. Master it. Then add another.
- Setting unrealistic deadlines: "Take all your pills perfectly for 30 days" is a recipe for failure. Try "7 out of 10 days this week." Build up.
- Not celebrating small wins: A patient who took their meds 6 out of 7 days? That’s progress. Say it. Write it down. Give a sticker. A diabetes educator shared that a simple sticker chart increased a patient’s weigh-ins from twice a week to five times a week.
- Ignoring tech fatigue: Older adults or people with cognitive challenges often abandon apps. Use low-tech tools: pill boxes, alarms on a basic phone, or family check-ins.
One nurse practitioner reported that 60% of her patients missed their first goal deadline-not because they didn’t try, but because the timeline was too tight. Adjusting from "one week" to "two weeks" cut missed deadlines in half.
Tools That Actually Help
You don’t need fancy tech. But if you have access to it, here’s what’s proven:
- Medisafe: A free app with reminders, pill identification, and sharing features for caregivers. Used by over 150,000 people. Rated 4.3 stars.
- Hero Smart Dispenser: Automatically dispenses pills at set times. Records doses. Sends alerts if skipped. Works without a smartphone.
- Smart pill bottles: AdhereTech, Hero, or NovoPen Echo for insulin. These sync with EHRs and give providers real-time data.
- Pharmacy apps: CVS, Walgreens, and others now offer refill reminders and adherence reports.
For clinics with limited resources, paper-based tracking with a weekly phone call is still effective. The goal isn’t the tool-it’s the conversation.
When SMART Goals Don’t Work
They’re not magic. If a patient has dementia, severe depression, or no social support, SMART goals alone won’t fix it. In those cases, you need caregivers involved. Or home visits. Or simplified regimens-like switching from three pills a day to one combined tablet.
Also, SMART goals don’t help in acute situations. If someone just had a heart attack and needs to take 12 pills right now, you don’t set goals-you give clear, repeated instructions and follow up daily.
But for chronic conditions-diabetes, high blood pressure, asthma, depression-SMART goals are the most effective tool we have. A 2022 study showed that every 10% increase in adherence cut heart failure readmissions by 5.7%.
Final Tip: Make It a Conversation, Not a Task
The best adherence programs don’t start with a checklist. They start with a question: "What’s the one thing you want to feel better about this month?" Then you build the goal around that. Maybe it’s sleeping through the night. Maybe it’s playing with your dog without getting tired. That’s the goal. The pills are just the tool.
When patients feel heard, they stick with it. When they feel lectured, they tune out. Your job isn’t to enforce compliance. It’s to help them find their own reason to stay on track.
What’s the most common mistake when setting medication adherence goals?
The biggest mistake is setting goals that are too broad or disconnected from the patient’s daily life. Saying "Take your pills every day" doesn’t help. People need specifics: what pill, when, where, and why it matters to them. Goals that match real habits-like taking meds after brushing teeth-stick much better than ones tied to abstract health outcomes.
Can I track medication adherence without using an app?
Absolutely. Many people, especially older adults, prefer simple methods. A printed calendar with stickers for each day taken, a pill box with compartments, or even a daily checklist on the fridge work well. The key is consistency and review-not technology. A weekly phone call from a nurse or family member can be just as effective as an app.
How long should I give someone to meet their adherence goal?
Start small. Two weeks is ideal for the first goal. That’s long enough to build a habit but short enough to feel achievable. After that, extend to four weeks, then monthly. If someone misses a goal, don’t punish them-ask why. Was the goal too hard? Did something change in their life? Adjust the plan together.
What if the patient doesn’t want to set goals?
Don’t push. Start with a conversation. Ask what they’re worried about. Maybe they’ve had bad experiences before. Maybe they feel judged. Listen first. Then say, "What’s one small thing you’d feel proud of if you did it this week?" Sometimes, just naming a tiny win-like taking one pill at the right time-builds trust. Goals come later.
Are SMART goals only for people with chronic illnesses?
No. They work for any long-term medication, including antibiotics after surgery, birth control, or even daily vitamins for someone with a deficiency. The key is whether the behavior needs to change over time. For short-term meds (like a 7-day course), simple reminders are enough. For anything lasting weeks or months, SMART goals help.
How do I know if my adherence tracking is working?
Look at two things: the number of doses taken and how the patient feels. If adherence improves and they report fewer symptoms-less dizziness, better sleep, more energy-you’re on the right track. Clinical data like HbA1c or blood pressure readings should also improve over time. If the numbers aren’t moving, revisit the goal. Maybe it’s not the right one.
Setting adherence goals isn’t about controlling patients. It’s about giving them control over their own health. When people see progress, even small wins, they keep going. And that’s how you turn a prescription into a lifestyle.
Fern Marder
December 2, 2025 AT 21:30OMG YES THIS!! 🙌 I used to forget my meds till I started linking them to my morning coffee. Now I take them right after I pour it-no app, no stress. Just coffee + pill = my new ritual. 🤘
Carolyn Woodard
December 3, 2025 AT 03:32The epistemological gap between self-reported adherence and objective tracking is staggering. One must interrogate the ontological assumptions underlying patient autonomy in therapeutic compliance-particularly when behavioral economics and neurocognitive load intersect with structural inequities in healthcare access.
Allan maniero
December 3, 2025 AT 09:16I've seen this work in my clinic-patients who set goals tied to their lives, not their diagnosis, stick like glue. One guy took his blood pressure med every time he checked his fantasy football stats. Weird? Maybe. Effective? Absolutely. The trick isn’t the pill-it’s the anchor in their routine.
Anthony Breakspear
December 4, 2025 AT 00:26Let’s be real-most doctors treat adherence like a math problem: take pill = good. But humans aren’t algorithms. You gotta meet people where they’re at. I had a patient who took her antidepressant after lighting her candle every night. Said it made her feel like she was choosing self-care, not just following orders. That’s the magic right there.
Zoe Bray
December 5, 2025 AT 22:39It is imperative to acknowledge that the implementation of SMART goal-based adherence protocols necessitates a multidisciplinary approach, incorporating clinical pharmacists, behavioral health specialists, and health informatics systems to ensure longitudinal fidelity and data integrity.
Girish Padia
December 6, 2025 AT 07:24People just need to stop being lazy. My grandpa took his pills every day without any apps or stickers. He just had discipline. Now everyone wants a trophy for taking medicine.
Saket Modi
December 7, 2025 AT 17:34Ugh. Another article telling us how to fix lazy people. Can we just make meds cheaper and less side-effecty? That’s the real problem.
Chris Wallace
December 9, 2025 AT 15:41I think what’s missing here is the emotional labor of adherence. It’s not just about remembering pills-it’s about showing up for yourself on days when you feel like nothing matters. That’s why the small wins matter so much. A sticker isn’t childish. It’s a lifeline.
william tao
December 11, 2025 AT 02:58SMART goals? More like SMART lies. The system is rigged. Pill costs are insane, insurance denies generics, and doctors don’t listen. You think a sticker chart fixes systemic neglect? Wake up.
Sandi Allen
December 12, 2025 AT 01:29Wait-so now we’re supposed to trust smart pill bottles? Who’s monitoring that data? Is Big Pharma watching when I open my bottle? What if they use it to raise prices? I’m not some lab rat for corporate surveillance!!
John Webber
December 13, 2025 AT 16:55i read this whole thing and the point is? take your pills when you do somthing every day. like brush your teeth. duh. why do we need 1000 words for that?
Shubham Pandey
December 14, 2025 AT 07:18Too much fluff. Just give them a pill box and call once a week. Done.
Elizabeth Farrell
December 15, 2025 AT 19:22I’ve worked with patients who thought their meds were pointless until we connected the dots: "Taking your insulin means you can carry your granddaughter without stopping to catch your breath." That’s not a clinical metric-that’s a human moment. And when you start there, the rest follows. No app needed. Just listening.