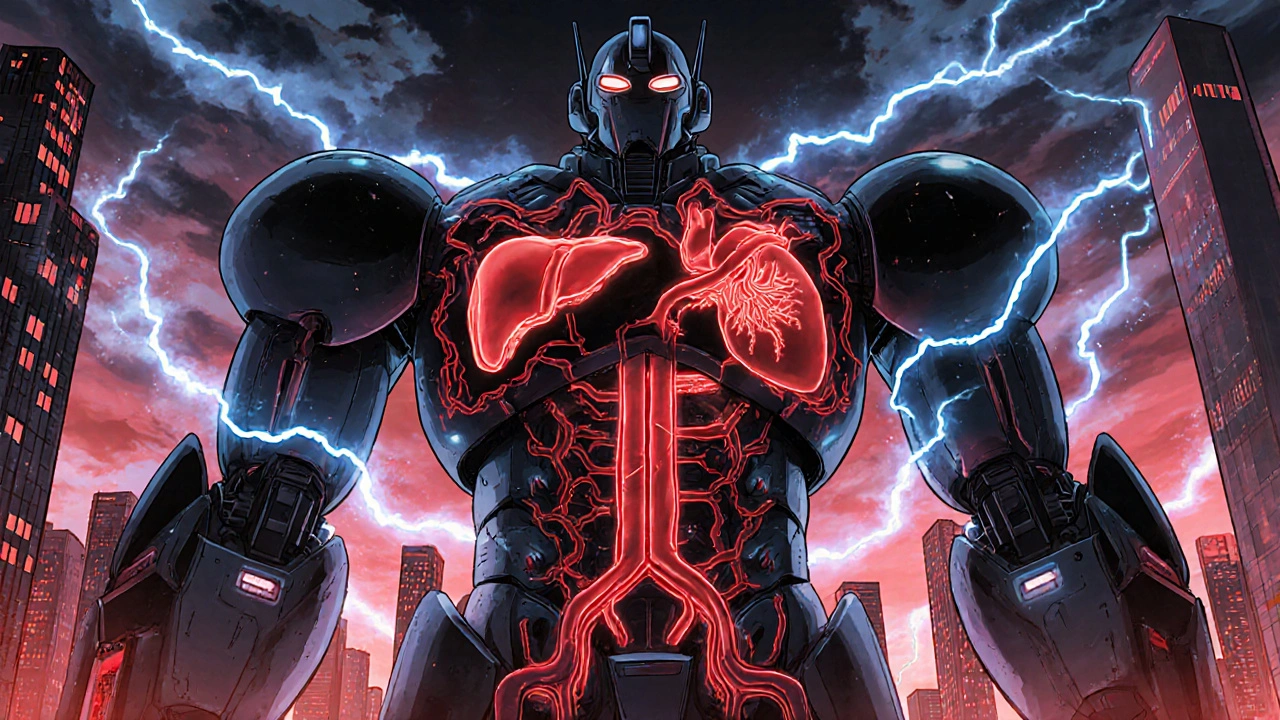
More than one in three adults in the U.S. has metabolic syndrome - and most don’t even know it. This isn’t just one problem like high blood pressure or high cholesterol. It’s a dangerous combo of five risk factors that work together to skyrocket your chance of a heart attack, stroke, or type 2 diabetes. If you’ve been told you have "a few things off" - high waist size, borderline glucose, or odd lipid numbers - this is what your doctor might be hinting at. And it’s not something you can fix with a pill. It’s a wake-up call that your lifestyle needs real change.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a disease on its own. It’s a cluster of conditions that happen together and make your heart and blood vessels work harder than they should. Think of it like a storm system: one rain cloud isn’t dangerous, but when five clouds gather over the same area, you get a hurricane.
To be diagnosed, you need at least three of these five specific markers:
- Abdominal obesity: Waist size over 40 inches for men, 35 inches for women (lower for Asian populations - 35 inches for men, 31 inches for women)
- High triglycerides: 150 mg/dL or higher
- Low HDL ("good" cholesterol): Under 40 mg/dL for men, under 50 mg/dL for women
- High blood pressure: 130/85 mmHg or higher
- Elevated fasting blood sugar: 100 mg/dL or higher
These numbers aren’t random. They’re based on decades of research from the American Heart Association and the National Institutes of Health. Having just one of these doesn’t mean much. But three? That doubles your risk of heart disease and makes you five times more likely to develop type 2 diabetes.
Why Insulin Resistance Is the Core Problem
At the heart of metabolic syndrome is insulin resistance - a condition where your muscle, fat, and liver cells stop responding properly to insulin, the hormone that shuttles sugar out of your blood and into your cells for energy.
Your pancreas tries to compensate by pumping out more insulin. This leads to hyperinsulinemia - high levels of insulin in your blood. Over time, this constant overdrive damages your blood vessels, raises your blood pressure, and makes your liver churn out more triglycerides while lowering your HDL. It’s a cascade effect.
And here’s the kicker: abdominal fat - the kind that wraps around your organs - is the main driver. Visceral fat isn’t just storage. It’s active tissue that releases inflammatory chemicals and free fatty acids directly into your liver, worsening insulin resistance. That’s why waist size matters more than overall weight. You can be "normal weight" and still have dangerous belly fat.
Why It’s Worse Than Individual Risk Factors
Doctors used to treat high blood pressure, high cholesterol, and high sugar as separate problems. But metabolic syndrome shows they’re connected. When these factors appear together, they don’t just add up - they multiply.
Think of it like a car with bad brakes, worn tires, and a faulty engine. Fixing one part helps, but if you don’t fix the others, the whole system is still at risk of crashing. Research from the Framingham Heart Study shows people with metabolic syndrome have a 1.5 to 2 times higher risk of cardiovascular events than those with just one or two of these factors.
It’s also a powerful predictor of diabetes. A 2007 meta-analysis found people with metabolic syndrome had over five times the risk of developing type 2 diabetes compared to those without it. That’s why the American Heart Association now calls it a "risk enhancer" - a red flag that you need more aggressive prevention, not just monitoring.

Who’s Most at Risk?
Metabolic syndrome doesn’t pick favorites - but it does favor certain groups.
- Ages 60+: Nearly half of adults over 60 have it, according to NHANES data.
- Hispanic and non-Hispanic Black populations: Prevalence is higher than in non-Hispanic whites - 38.6% and 31.8% respectively.
- People with PCOS: Up to 70% of women with polycystic ovary syndrome have insulin resistance and meet criteria for metabolic syndrome.
- Those with sedentary jobs or diets high in refined carbs: Sugar and white bread spike insulin repeatedly, training your body to resist it.
And it’s getting worse. Between 1999 and 2018, the percentage of U.S. adults with abdominal obesity jumped from 46% to nearly 60%. The same trend is now visible in countries like India, Brazil, and Mexico, where fast food and sugary drinks have replaced traditional diets.
What You Can Do - And What Doesn’t Work
There’s no pill for metabolic syndrome. No drug has been approved to treat the whole cluster. That’s because the solution isn’t chemical - it’s behavioral.
The Diabetes Prevention Program (DPP), a landmark NIH study, proved that lifestyle change works better than medication. Participants who lost 7% of their body weight through diet and 150 minutes of walking per week reduced their risk of developing diabetes by 58%. Even better - 41% of them reversed metabolic syndrome entirely within 10 years.
Here’s what actually helps:
- Weight loss: Losing just 5-10% of your body weight can normalize blood pressure, lower triglycerides, and improve insulin sensitivity.
- Move daily: Walking 30 minutes a day, five days a week, is enough to start reversing the damage. Strength training twice a week helps too - muscle burns sugar better than fat.
- Eat real food: Cut out sugary drinks, white bread, pastries, and processed snacks. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats like olive oil and avocado.
- Sleep and stress matter: Poor sleep and chronic stress raise cortisol, which increases belly fat and insulin resistance. Aim for 7-8 hours of sleep. Try breathing exercises or walking in nature to lower stress.
What doesn’t work? Crash diets. Starvation. Weight-loss pills that promise quick fixes. These often backfire, leading to muscle loss, slowed metabolism, and weight regain - which makes insulin resistance worse.

Why Many People Are Misdiagnosed
Here’s the ugly truth: most people with metabolic syndrome are never told they have it.
On HealthUnlocked, 68% of users said their doctor only addressed one issue - like high blood pressure - and never connected the dots. One Reddit user wrote: "I had high triglycerides for years. My doctor gave me a statin. Then I got prediabetes. Then my BP went up. No one said, ‘You have metabolic syndrome.’"
Doctors are busy. They’re trained to treat individual numbers, not patterns. But if you have two or more of these risk factors, you should ask: "Could this be metabolic syndrome?"
And if you’re diagnosed, don’t accept fragmented care. Seek out a team: a dietitian, a physical therapist, and a primary care provider who understands the whole picture. Programs like the Mayo Clinic’s Integrated Metabolic Syndrome Program have shown that with coordinated care, 68% of patients reverse the syndrome in a year.
New Tools Are Making a Difference
In 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. It uses continuous glucose monitoring (CGM) paired with AI-driven coaching to help users understand how food affects their blood sugar in real time.
In a clinical trial, users saw their HbA1c drop by 0.6% and their waistline shrink by 3.2 cm in six months - without medication. That’s the power of feedback. When you see your blood sugar spike after a bagel, you’re far more likely to skip it next time.
Researchers are also exploring genetic markers like PNPLA3 and TM6SF2 that might predict who responds best to low-fat vs. low-carb diets. This could lead to truly personalized plans in the next five years.
Hope Is Real - And It Starts Today
The DiRECT trial in the UK showed that 46% of people with type 2 diabetes and metabolic syndrome achieved full remission after losing 15 kg or more through a structured low-calorie diet and long-term support. Their blood sugar returned to normal. Their triglycerides dropped. Their blood pressure normalized. They stopped taking all diabetes meds.
That’s not a miracle. That’s science. And it’s possible for you too - if you start now.
You don’t need to run a marathon. You don’t need to buy expensive supplements. You just need to move more, eat real food, and give your body a chance to heal. The numbers don’t lie - and neither does your body. If you’ve been ignoring those "minor" lab results, it’s time to listen. Your heart is waiting.
Can you have metabolic syndrome without being overweight?
Yes. While abdominal fat is the main driver, some people - especially those with genetic predispositions or conditions like PCOS - can have insulin resistance and metabolic syndrome even if their overall weight is normal. Waist size is a better indicator than BMI. If your waist is over 35 inches (women) or 40 inches (men), you’re at risk regardless of your weight.
Does metabolic syndrome always lead to diabetes?
No, but it greatly increases the risk. About 75-80% of new type 2 diabetes cases are linked to metabolic syndrome. However, lifestyle changes can prevent or delay it. The Diabetes Prevention Program showed that 58% of people avoided diabetes with diet and exercise alone. Early action makes all the difference.
Are medications used to treat metabolic syndrome?
There’s no drug approved to treat metabolic syndrome as a whole. But doctors may prescribe medications for individual components: statins for high cholesterol, ACE inhibitors for high blood pressure, or metformin for elevated blood sugar. These help manage symptoms, but they don’t reverse the root cause - insulin resistance. Lifestyle change remains the only proven way to reverse the syndrome.
How long does it take to reverse metabolic syndrome?
Significant improvement can happen in 3-6 months with consistent effort. Losing 5-10% of your body weight, exercising 150 minutes per week, and eating whole foods can normalize blood pressure, triglycerides, and fasting glucose. Full reversal - where all five criteria fall below diagnostic thresholds - often takes 6-12 months. The key is consistency, not speed.
Is metabolic syndrome reversible?
Absolutely. Multiple studies, including the Diabetes Prevention Program and the DiRECT trial, show that metabolic syndrome can be reversed through weight loss, physical activity, and dietary changes. Many people not only reverse the syndrome but also stop taking medications for high blood pressure, cholesterol, or prediabetes. It’s not easy, but it’s possible - and it saves lives.
Jefriady Dahri
November 23, 2025 AT 16:33Man, I never realized how many people are walking around with this silent killer inside them. I had high triglycerides last year and thought it was just a fluke. Turns out I had three of the five markers. Started walking 30 mins a day and cutting soda. Lost 12 lbs in 3 months. My doc was shocked. You don’t need a miracle, just consistency. 💪
Andrew McAfee
November 25, 2025 AT 05:01So basically its just sugar and sitting down thats killing us and nobody wants to admit it
Andrew Camacho
November 25, 2025 AT 23:09Oh wow another ‘lifestyle change’ lecture. Tell me something I don’t know. Meanwhile Big Pharma is laughing all the way to the bank selling statins and metformin to people who just need to stop eating Twinkies. But nooo, let’s blame the victim while the food industry gets tax breaks. This whole thing is a distraction. You think your grandma’s fried chicken is the problem? Nah. It’s the corn syrup in everything. And the government subsidizes it. Wake up.
Arup Kuri
November 26, 2025 AT 10:23They dont tell you this but its all about the GMOs and the fluoride in the water. I saw a video on YouTube where they showed how insulin resistance starts after 3 months of drinking city water. Your body is being poisoned. Stop trusting doctors. They get paid by the pharma companies. Eat raw garlic and jump rope at dawn. Thats the real fix.
Elise Lakey
November 27, 2025 AT 22:55I’ve been told I have prediabetes and high blood pressure but no one ever said ‘metabolic syndrome.’ I didn’t even know these things were connected. This post made me feel less alone. I’m scared but also hopeful. I’m going to start with just walking after dinner. Small steps, right?
Erika Hunt
November 28, 2025 AT 08:23It’s fascinating how the body responds to chronic insulin spikes-it’s not just about calories in, calories out, it’s about hormonal signaling, cellular communication, inflammatory pathways, adipokine secretion, mitochondrial dysfunction, and gut microbiome modulation-all of which are interwoven in a way that makes metabolic syndrome not just a collection of symptoms, but a systemic dysregulation that requires a systems-level approach, not just a pill for each number.
Sharley Agarwal
November 29, 2025 AT 11:45People who ignore this deserve what they get.
prasad gaude
November 30, 2025 AT 11:59You know, in India we used to eat roti, dal, and greens. Now it’s pizza and bhelpuri with extra sugar. My uncle had all five markers-he was 58, thin, but had a belly like a pregnant woman. He started walking to the temple every morning. No meds. Just movement, silence, and a little turmeric milk. Two years later, his labs were normal. Sometimes healing isn’t about science. It’s about rhythm.
Timothy Sadleir
December 2, 2025 AT 10:38While it is undeniably true that lifestyle modifications constitute the primary therapeutic modality in the context of metabolic syndrome, one must not overlook the fact that the prevalence of this condition is inextricably linked to the commodification of nutrition, the erosion of public health infrastructure, and the systemic failure of regulatory bodies to enforce evidence-based dietary guidelines. The individual bears responsibility, yes-but the structural environment is the true vector of pathology.
Srikanth BH
December 3, 2025 AT 16:00You got this. I was in the same spot-high waist, high sugar, low HDL. Started with one change: swapped soda for sparkling water. Then added 10-minute home workouts. Didn’t go all-in. Just did a little every day. Now I’m off all meds. It’s not about being perfect. It’s about showing up. You’re already ahead by reading this.
Jennifer Griffith
December 4, 2025 AT 01:35so like… if i eat avocado toast every day am i doomed??
Roscoe Howard
December 4, 2025 AT 15:09It’s not just diet. It’s the decline of American work ethic. In my day, people walked to work. Now they sit in air-conditioned offices and blame ‘stress.’ We used to eat real food. Now it’s processed nonsense imported from China. This isn’t a health crisis-it’s a cultural surrender. And no app is going to fix that.
Andrew Camacho
December 5, 2025 AT 03:15Oh so now the solution is ‘walk more’? That’s rich. I work two jobs, have three kids, and my wife’s on dialysis. You think I’ve got time to ‘eat real food’? Your privilege is showing. Meanwhile, the cheapest food in the store is the stuff that’s killing us. And you’re telling me to ‘just change’? Try surviving on SNAP and then talk to me about lifestyle.
Kimberley Chronicle
December 5, 2025 AT 06:07Interesting that the DiRECT trial used a low-calorie formula diet-structured, supervised, and time-limited. The key variable wasn’t just weight loss, but the degree of fat mass reduction in the liver and pancreas, which restored beta-cell function. This suggests a biological threshold for reversal, not merely behavioral adherence. The real challenge is scalability: can this be replicated in primary care without specialist support?