Acute Kidney Injury (AKI) doesn’t announce itself with a siren. It creeps in quietly-maybe after a bad bout of food poisoning, a hospital stay, or even just skipping fluids on a hot day. One day your body feels fine; the next, you’re exhausted, swollen, and confused. By the time symptoms show up, your kidneys may already be struggling. AKI isn’t just a lab value gone wrong. It’s your body screaming that something’s seriously off-and time is running out.
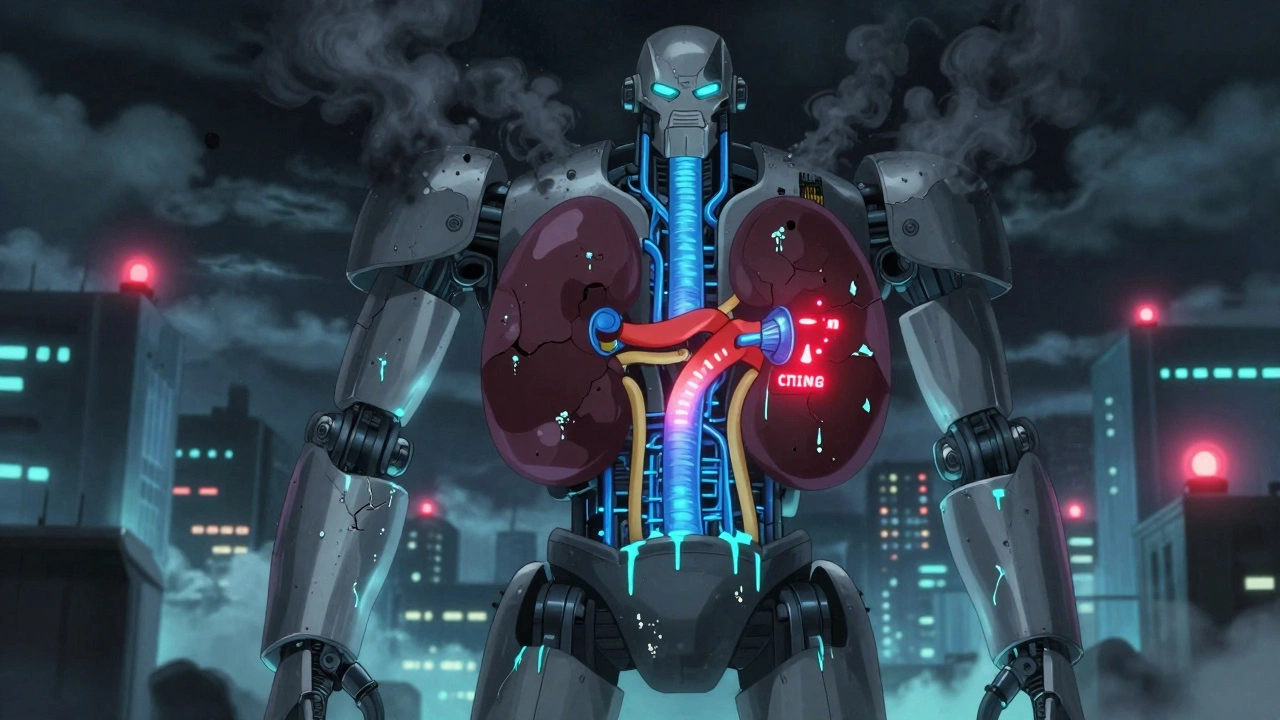
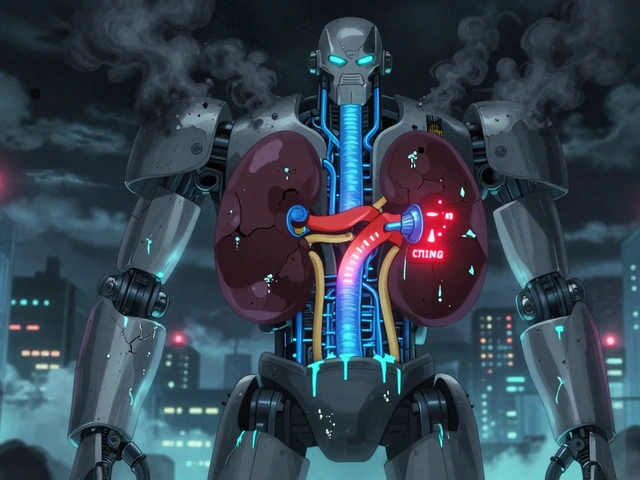
What Happens When Your Kidneys Shut Down
Your kidneys don’t just make urine. They filter toxins, balance electrolytes, control blood pressure, and keep your blood chemistry stable. When AKI hits, that system collapses fast. The official definition? A sudden drop in kidney function over hours or days. This shows up as a spike in serum creatinine-usually by at least 0.3 mg/dL in 48 hours-or a big drop in urine output. Some people stop peeing altogether. Others? They still urinate normally, but their kidneys are still failing. That’s why lab tests matter more than symptoms.What makes AKI dangerous isn’t just the kidney damage itself. It’s what happens next. Fluid builds up in your lungs, making it hard to breathe. Potassium leaks into your bloodstream, risking a heart rhythm that can stop you dead. Acid piles up in your blood. Your body starts poisoning itself with waste it can’t flush out. And here’s the kicker: about 1 in 5 people with AKI have no symptoms at all. They’re found by accident during routine blood work. That’s why hospitals now flag rising creatinine levels automatically-because waiting for symptoms means waiting too long.
Why Your Kidneys Stopped Working
AKI doesn’t happen for no reason. It’s almost always tied to one of three causes-and knowing which one changes everything.Prerenal AKI (60-70% of cases) means your kidneys aren’t getting enough blood. This isn’t a kidney problem-it’s a circulation problem. Severe dehydration from vomiting or diarrhea? Check. Major blood loss? Check. Low blood pressure from infection or heart failure? Check. Your kidneys are fine, but they’re starving. Give them fluids, and they often bounce back fast. In fact, 70% of these cases recover fully if treated within 24 hours.
Intrarenal AKI (25-35%) is where the damage is inside the kidney itself. The most common culprit? Acute tubular necrosis (ATN). This happens when kidney cells die from toxins or lack of oxygen. Common triggers? Antibiotics like gentamicin, contrast dye used in CT scans, or even some painkillers taken in high doses. Glomerulonephritis-where the kidney’s filtering units get inflamed-also falls here. This type is trickier. Recovery takes weeks, and sometimes the damage sticks around.
Postrenal AKI (5-10%) is all about blockage. If urine can’t leave your body, pressure backs up into your kidneys and crushes them. In men over 60, it’s often an enlarged prostate. In others, it’s kidney stones, tumors, or even blood clots in the ureters. The good news? Once you remove the blockage-usually with a stent or catheter-kidney function often snaps back within days. Speed matters here. The longer the blockage lasts, the less likely full recovery becomes.
The Warning Signs You Can’t Ignore
Symptoms vary wildly. Some people feel fine until they collapse. Others are screaming for help. Here’s what to watch for:- Urine output drops below 400 mL a day-or stops entirely.
- Swelling in legs, ankles, or face from fluid buildup.
- Shortness of breath, even when sitting still.
- Extreme fatigue, dizziness, or confusion-especially in older adults.
- Nausea, vomiting, or loss of appetite.
- Flank pain (back pain just below the ribs).
- Chest pain from inflammation around the heart.
But here’s the trap: many of these look like other problems. Fatigue? Could be stress. Swelling? Could be heart issues. Confusion? Could be dementia. That’s why doctors don’t rely on symptoms alone. They check creatinine. They look at urine output. They order an ultrasound to rule out blockages. If your creatinine jumped from 0.9 to 1.8 in a week? That’s not normal. That’s AKI.

How Doctors Diagnose It
There’s no single test for AKI. It’s a puzzle solved with blood, urine, and imaging.First, they check serum creatinine. Normal levels? Around 0.6 to 1.2 mg/dL for women, 0.7 to 1.3 for men. A rise of 0.3 mg/dL in 48 hours? That’s stage 1 AKI. A tripling of your baseline? That’s stage 3-the most serious. They also check BUN (blood urea nitrogen). High BUN with low urine output? Classic sign.
Then they look at urine. A low sodium level in urine (FeNa under 1%) suggests prerenal AKI. High sodium (over 2%)? Likely intrinsic damage. They may also test for new biomarkers like NGAL or TIMP-2/IGFBP7, which can warn of AKI 24 to 48 hours before creatinine rises. These aren’t routine yet, but they’re becoming more common in ICUs.
An ultrasound is almost always done. It shows if the kidneys are swollen, if there’s a blockage, or if they’ve shrunk from chronic damage. A CT scan with contrast? Risky if you’re already at risk for AKI. Doctors avoid it unless absolutely necessary.
Treatment: Fix the Cause, Not Just the Numbers
You don’t treat AKI with one magic pill. You treat the reason it happened.If it’s prerenal? Fluids. Fast. A liter or two of IV saline, and many patients improve within hours. No more dehydration. No more low blood pressure. Kidneys wake up.
If it’s drug-induced? Stop the drug. Immediately. Antibiotics, NSAIDs, contrast dye-any of these could be the trigger. Discontinuing the toxin leads to recovery in 65% of cases within 3 days.
If there’s a blockage? Remove it. A stent in the ureter. A catheter for an enlarged prostate. In 90% of cases, kidney function returns within 48 hours.
If the damage is deep? That’s where things get serious. You might need dialysis. Not because it fixes the kidney-but because it buys time. Hemodialysis three times a week. Or CRRT (continuous dialysis) in the ICU, which is gentler for unstable patients. About 5-10% of hospitalized AKI patients need this. And yes, it’s life-saving. But it’s not a cure.
For autoimmune causes like glomerulonephritis? Immunosuppressants-steroids, cyclophosphamide. For hemolytic uremic syndrome? Plasmapheresis. These are targeted, powerful treatments. And they work best when started fast.
Recovery: It’s Not Guaranteed
Some people bounce back fully. Others never do.Prerenal AKI? 70-80% recover completely in a week or two. No long-term damage.
Intrarenal AKI? Only 40-60% fully recover. If you had prolonged low urine output-more than two weeks-your chances drop to 20-30%. Age matters. If you’re over 65? Your recovery rate drops by 35%. If your kidneys were already weak before? Your odds halve.
And here’s the quiet crisis: 23% of AKI survivors develop chronic kidney disease within a year. Each episode of AKI increases your risk of needing dialysis fivefold over the next five years. Even if your creatinine looks normal now, your kidneys might be scarred. That’s why follow-up is non-negotiable. You need blood tests at 3 months, 6 months, and a year. A nephrologist should see you.

The Hidden Toll: More Than Just Physical
Recovery isn’t just about numbers. It’s about energy, anxiety, and fear.A 2022 survey of over 1,200 AKI survivors found that 68% felt exhausted for months-even after their labs normalized. 42% had constant anxiety about their kidneys. One man described it: "I could walk 50 feet and collapse. I was terrified I’d need dialysis forever." That’s not weakness. That’s trauma.
People lose jobs. They can’t exercise. They stop socializing. The mental load is heavy. And it’s rarely talked about. Recovery isn’t just a lab result. It’s rebuilding your life.
What You Can Do
If you’re at risk-diabetic, elderly, on blood pressure meds, or recently hospitalized-here’s what to do:- Stay hydrated. Especially if you’re sick with vomiting or diarrhea.
- Avoid NSAIDs like ibuprofen or naproxen unless your doctor says yes.
- Know your baseline creatinine. Ask your doctor for a copy of your last blood test.
- Speak up if you feel unusually tired, swollen, or confused.
- After hospital discharge, schedule a follow-up blood test in 1-2 weeks.
AKI isn’t something you can ignore. But it’s also not a death sentence. It’s a warning. And if you catch it early, you can stop it from becoming permanent.
Can you fully recover from acute kidney injury?
Yes, many people fully recover, especially if the cause is prerenal-like dehydration or low blood pressure-and it’s treated quickly. Around 70-80% of these cases bounce back within a week. But if the injury is inside the kidney (like from toxins or infection) or lasts more than a week, recovery is less certain. About 40-60% of those cases improve, but some are left with lasting damage. Age, prior kidney problems, and needing dialysis lower your chances of full recovery.
How long does it take to recover from acute kidney injury?
Recovery time depends on the cause. Prerenal AKI often improves in 24 to 48 hours with fluids. Intrarenal AKI, like from acute tubular necrosis, can take 2 to 6 weeks. If you’re on dialysis, recovery might take months-or may not happen at all. Some people see creatinine levels normalize in days but still feel exhausted for 3 to 6 months. The body needs time to heal, even after the kidneys start working again.
Can AKI come back after recovery?
Yes. Once you’ve had AKI, your kidneys are more vulnerable. Each episode increases your risk of future injury. People who’ve had AKI are 8 times more likely to develop end-stage kidney disease within 5 years. That’s why avoiding dehydration, checking meds, and monitoring blood pressure is critical-even years later. Your kidneys never fully forget the trauma.
Is AKI the same as chronic kidney disease?
No. AKI is sudden and often reversible. Chronic kidney disease (CKD) is gradual damage that lasts longer than 3 months. But AKI can lead to CKD. About 23% of AKI survivors develop stage 3 or worse CKD within a year. Think of AKI as a sharp injury, and CKD as the scar that remains. Preventing repeat AKI is one of the best ways to avoid long-term kidney failure.
What medications should I avoid after AKI?
Avoid NSAIDs like ibuprofen, naproxen, or high-dose aspirin-they reduce blood flow to kidneys. Some antibiotics (like gentamicin), contrast dye used in imaging, and certain blood pressure meds (ACE inhibitors or ARBs) can also be risky, especially if you’re dehydrated. Always check with your doctor before taking any new medication-even over-the-counter ones. Your kidneys are more sensitive now.
Do I need to see a kidney specialist after AKI?
Yes, if you had moderate to severe AKI-or if you’re over 65, diabetic, or had high blood pressure before-you should see a nephrologist within 6 months. Even if your creatinine is normal now, your kidneys may have hidden scarring. A specialist can track your kidney function, check for protein in urine, and help prevent future damage. One in two AKI survivors needs this follow-up.
What’s Next for AKI Treatment
The future is about catching AKI before it happens. New blood tests can spot kidney stress 24 hours before creatinine rises. AI tools are being trained to predict AKI by analyzing electronic records-flagging patients at risk before they even feel sick. Clinical trials are testing whether starting dialysis earlier saves lives. And research into kidney repair mechanisms could one day lead to drugs that help damaged cells heal themselves.For now, the message is simple: don’t wait for symptoms. Know your numbers. Protect your kidneys. And if you’ve had AKI-treat your body like it’s still healing. Because it is.
John Fred
December 13, 2025 AT 13:42Bro, AKI is no joke 😰 I saw my dad go through this after a bad UTI turned into sepsis. They caught it early because his creatinine spiked from 1.1 to 2.4 in 36 hours. Fluids, stat. He was back to golfing in 10 days. Prerenal = easy fix if you don’t sleep on it 🚨💧
Harriet Wollaston
December 14, 2025 AT 13:26This hit me right in the feels. My mom had AKI after her chemo and I didn’t even know what it was until she was in the ICU. She’s fine now, but the fatigue? Still there after 8 months. It’s not just ‘get better’-it’s like your body remembers the trauma. Thank you for saying that. 💛
Lauren Scrima
December 15, 2025 AT 14:00So… you’re telling me NSAIDs are the villain here? 🙄 Like, I thought ibuprofen was just ‘harmless pain relief’? Thanks for the wake-up call. Also, ‘creatinine jumped from 0.9 to 1.8’? That’s not a ‘slight bump’-that’s your kidneys screaming into a pillow. 😤
Tommy Watson
December 15, 2025 AT 14:00lol i read this whole thing and still dont get why my cousin died from 'kidney thing' after a flu. they said it was 'akie' or whatever. why didnt they just fix it? they gave him water and then he was gone. rip. 😭
Richard Ayres
December 16, 2025 AT 20:48This is one of the most clinically accurate and humanely written pieces on AKI I’ve read in years. The distinction between prerenal, intrarenal, and postrenal is critical for both clinicians and patients. I especially appreciate the emphasis on follow-up-many primary care providers overlook this. The data on 23% developing CKD within a year is alarming and under-discussed. Thank you for raising awareness.
Michael Gardner
December 18, 2025 AT 14:1970% recover? That’s a lie. My neighbor had prerenal AKI, got fluids, ‘recovered’-then ended up on dialysis 18 months later. They always say ‘it’s reversible’ until it’s not. The system’s lying to us to make us feel better. This isn’t a medical issue-it’s a corporate one. Dialysis is profitable.
Willie Onst
December 18, 2025 AT 14:48You know, I used to think kidneys were just… plumbing. But this? This is like your body’s internal orchestra. One instrument goes out of tune, and the whole symphony collapses. And no one tells you until the music stops. I’m gonna start drinking water like it’s my job now. 🙏💧
Jennifer Taylor
December 20, 2025 AT 05:13CONSPIRACY: Hospitals *want* you to have AKI so they can bill for dialysis. They don’t tell you that contrast dye is poison. They don’t tell you that your ‘routine blood work’ is a trap. They’re selling you a slow death with a side of insurance claims. 🕵️♀️💉 #AKIisABusiness
nithin Kuntumadugu
December 21, 2025 AT 21:24u think ur kidneys are important? in india we dont even have labs to check creatinine. people die from AKI in villages and no one knows why. u rich americans worry about NSAIDs? we worry about drinking dirty water. this post is so privileged. 🤡