When it comes to getting affordable prescription drugs through Medicaid, what you get isn’t the same everywhere. Even though every state covers generic medications under Medicaid, the rules, costs, and restrictions vary wildly-from one state line to the next. A person in Colorado might need to try five other drugs before their doctor can approve the one they need, while someone in California might walk into a pharmacy and get the same generic with no paperwork at all. This isn’t just about bureaucracy. It’s about whether someone with diabetes, high blood pressure, or asthma can actually afford to stay on their medication.
What Medicaid Covers: The Federal Floor
Federal law doesn’t require states to cover prescription drugs, but every single state does. Why? Because the financial incentive is too strong. The Medicaid Drug Rebate Program, created in 1990, forces drug manufacturers to pay rebates to states in exchange for including their drugs on Medicaid formularies. In 2024, generic drugs made up 84.7% of all Medicaid prescription claims, and they cost far less than brand-name drugs. That’s why states rely on them so heavily: they saved $38.7 billion in federal fiscal year 2024 alone.
But here’s the catch: federal law still bans coverage for certain drugs-like those for weight loss, fertility, or cosmetic use. Beyond that, states have almost complete freedom to decide which generics to cover, how much patients pay, and how tightly they control access.
Generic Substitution: Automatic or Not?
Forty-one states require pharmacists to substitute a generic drug for a brand-name version if it’s listed as therapeutically equivalent by the FDA. That means if your doctor prescribes Lipitor, and there’s a generic version of atorvastatin, the pharmacist must give you the generic unless you or your doctor say no.
But not all states are that strict. In some places, substitution is allowed-but not required. In others, like Colorado, the law goes further: if a generic is cheaper and equally effective, the prescriber must write for it, unless there’s a documented reason not to. For example, if a patient has been stable on a brand-name drug for months, switching could cause a relapse. In those cases, the doctor can override the substitution rule.
Even more confusing? Twenty-eight states require the pharmacist to document why they substituted a drug. Twelve states don’t require any notice to the prescriber at all. That means a patient might get a different generic than expected, and their doctor won’t even know.
Copays: Paying More Than You Think
Most people assume Medicaid is free. But many states charge copays-even for generics. The federal limit? Up to $8 per prescription for people earning below 150% of the federal poverty level. But here’s the twist: some states charge nothing. Others charge $1, $3, or $5. And it’s not always the same drug.
States use tiered formularies to control costs. Tier 1 is usually generics, with the lowest copay. Tier 2 is brand-name drugs, with higher costs. But even within Tier 1, some states make certain generics “non-preferred.” That means you pay more for them-even if they’re chemically identical to the preferred version.
For example, a patient in Texas might pay $1 for a common blood pressure generic, but $5 for another generic that’s equally effective. Why? Because the state’s pharmacy benefit manager (PBM) negotiated a better deal on the first one. The patient doesn’t get a say. And if they can’t afford the $5, they might skip their refill.
Prior Authorization: The Hidden Bureaucracy
Some states don’t stop at copays or substitution rules. They add another layer: prior authorization. This means your doctor has to call, fax, or submit an online form to prove you need the drug before Medicaid will pay for it.
Colorado’s Health First Colorado program is one of the strictest. For certain gastrointestinal drugs, you must have tried three different proton pump inhibitors and all preferred NSAIDs at maximum doses before they’ll approve a new one. That’s not just paperwork-it’s months of trial and error, often with worsening symptoms.
On the other end, California’s Medi-Cal program rarely requires prior authorization for generics. The difference? It’s not about medical necessity-it’s about how aggressively a state is trying to cut costs.
And the wait times? They vary too. In Colorado, decisions come in under 24 hours. In some states, it takes up to 72 hours. For someone with a chronic condition, that delay can mean a hospital visit.
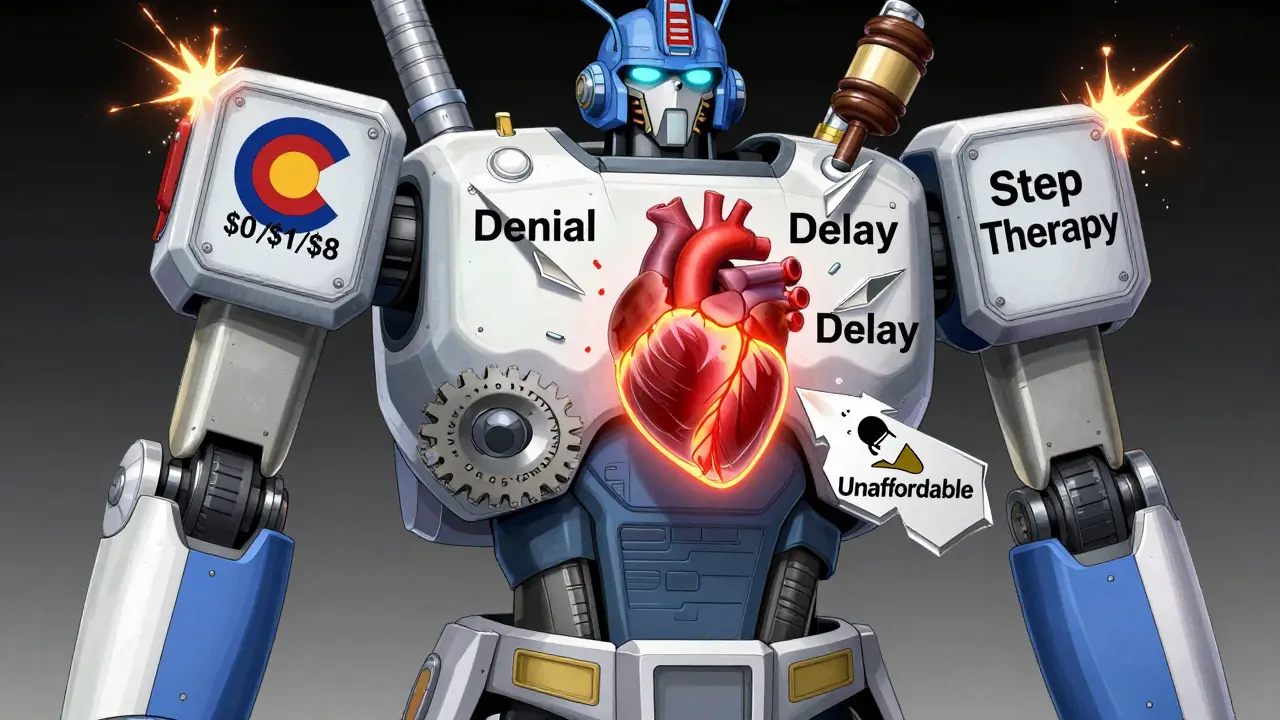
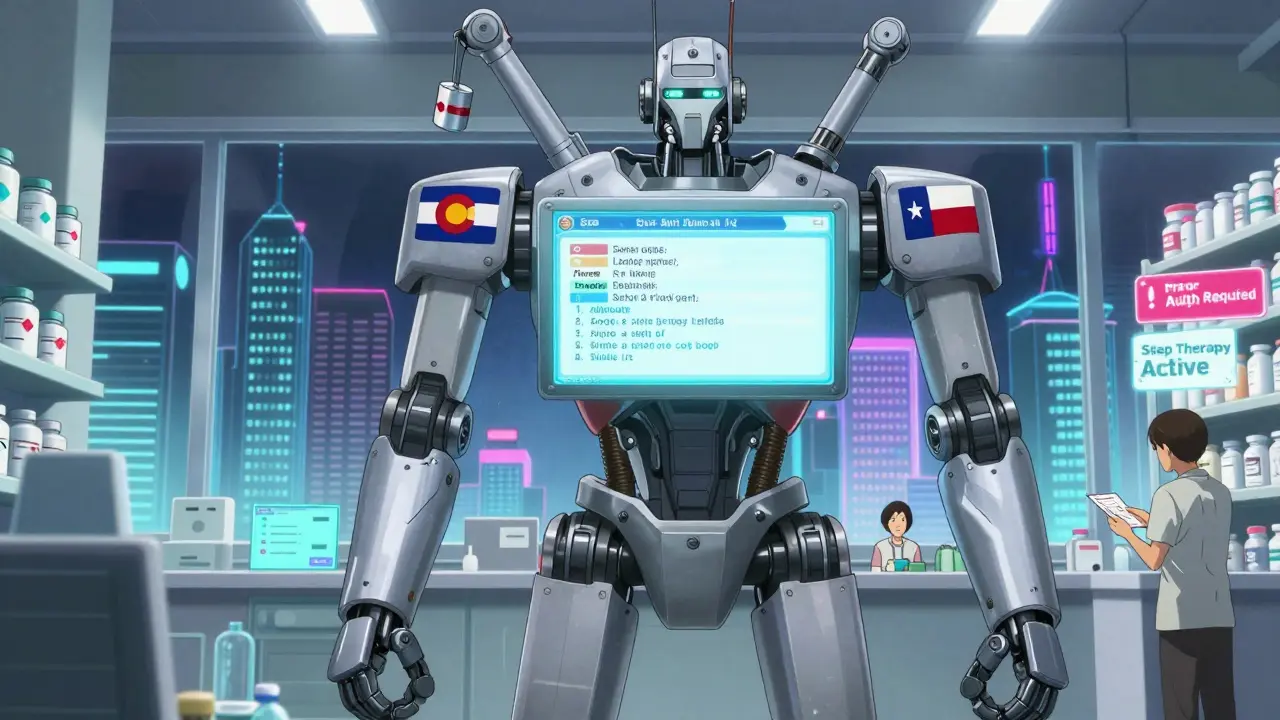
Formularies and Step Therapy: What You Can and Can’t Get
Thirty-two states use step therapy-also called “fail first.” That means you have to try the cheapest, most common drug before you can get a more expensive one-even if your doctor says it won’t work for you.
For example, if you have rheumatoid arthritis, you might be forced to try methotrexate before they’ll approve a biologic-even if you’ve already tried it and it caused serious side effects. In states without step therapy, your doctor’s judgment is respected.
These formularies aren’t just lists. They’re living documents updated every few months. CVS Caremark, Express Scripts, and OptumRx manage pharmacy benefits for 37 states. Each has its own rules, and each updates its list independently. A drug covered in New York might be excluded in Florida. And if you move? You might lose access overnight.
The Human Cost of Fragmentation
This patchwork system doesn’t just frustrate doctors-it harms patients. A 2024 University of Pennsylvania study found that when Medicaid patients were denied a drug due to prior authorization, their risk of hospitalization jumped by 12.7%. That’s not just a statistic. It’s someone in pain, skipping doses, or going without.
Primary care doctors spend an average of 15.3 minutes per patient just navigating prior authorization systems. That’s over 8,200 hours a year per doctor-time that could’ve been spent on care, not paperwork. And for community pharmacies, reimbursement rates determine whether they even participate. In Vermont, 98% of pharmacies accept Medicaid. In Texas, it’s only 67%. That means rural patients might have to drive 50 miles to fill a prescription.
What’s Changing in 2025 and Beyond
New rules are coming. In December 2024, CMS proposed requiring all Medicaid programs to cover anti-obesity medications. If approved, it would affect nearly 5 million people. But it’s also creating tension. States argue they can’t afford it without more federal funding.
Meanwhile, Congress is considering a bill that would remove inflation-based rebates for most generic drugs. If it passes, states could lose $1.2 billion a year in rebates. That could mean higher copays, tighter formularies, or even drug exclusions.
And here’s something few realize: people on Medicaid can now switch their Medicare drug plan once a month. That’s great for those with dual eligibility-but it adds another layer of confusion. A drug covered under Medicaid today might not be covered under Medicare tomorrow.

What Patients and Providers Need to Know
If you’re on Medicaid:
- Check your state’s Preferred Drug List (PDL) every few months-it changes often.
- Ask your pharmacist: “Is this the preferred generic?” If not, ask why.
- If you’re denied a drug, request a written explanation. You have the right to appeal.
- Call your state’s Medicaid office directly. Their website won’t always tell you the full story.
If you’re a provider:
- Know your state’s substitution laws. Some require documentation. Others don’t.
- Use tools like the Medicaid Formulary Lookup (available in 34 states) to check coverage before prescribing.
- Document therapeutic reasons for prescribing brand-name drugs-even if they’re more expensive.
- Advocate for your patients. Many denials are overturned with a simple phone call.
| State | Generic Substitution Required? | Max Generic Copay | Prior Authorization for Generics? | Step Therapy Used? |
|---|---|---|---|---|
| Colorado | Yes | $8 | Yes (for non-preferred) | Yes |
| California | Yes | $1 | Rarely | No |
| Texas | Yes | $5 | Yes | Yes |
| Massachusetts | Yes | $0 | Minimal | Yes |
| Vermont | Yes | $0 | No | No |
| Mississippi | Yes | $8 | Yes | Yes |
Frequently Asked Questions
Are all generic drugs covered by Medicaid?
No. While Medicaid covers most generic drugs, states can exclude certain ones from their formulary based on cost, safety, or clinical guidelines. Some states exclude generics that have recently entered the market or that don’t meet specific cost-effectiveness thresholds. Always check your state’s current Preferred Drug List.
Can I get a brand-name drug instead of a generic if I prefer it?
Yes-but only if your doctor provides a medical reason. In states with mandatory substitution, you can request a brand-name drug if the generic caused side effects, isn’t effective for you, or if you’re already stable on the brand. You’ll need documentation from your provider. Some states require prior authorization even for brand-name drugs in these cases.
Why do some pharmacies refuse to fill my Medicaid prescription?
Some pharmacies opt out of Medicaid because the reimbursement rate is too low to cover their costs. In states like Texas, only about two-thirds of pharmacies accept Medicaid. If your local pharmacy refuses, ask if they’re contracted with your state’s PBM. You can also use mail-order services or find another pharmacy through your state’s Medicaid website.
What happens if I move to another state?
Your coverage changes immediately. A drug covered in one state might be excluded in another. You’ll need to reapply for Medicaid in your new state and get a new formulary. Some drugs may require prior authorization or step therapy that didn’t exist before. Always contact your new state’s Medicaid office before moving if you rely on ongoing medication.
Can pharmacists switch my generic without telling me?
In 12 states, pharmacists can substitute generics without notifying your doctor or you. In 28 others, they must document the change. Always ask if your prescription was switched. Even if it’s the same drug, different manufacturers can have different fillers or release mechanisms that affect how well it works for you.
Is there a way to appeal a denial of a generic drug?
Yes. Every state has a formal appeals process. You or your doctor can submit a written request for reconsideration. Many denials are overturned on appeal, especially if your provider includes clinical evidence. The process usually takes 7-14 days for standard appeals and 72 hours for urgent cases. Don’t give up-this is your right.
What’s Next?
The system isn’t broken-it’s overloaded. States are trying to balance affordability with access, but the tools they use-copays, prior auth, step therapy-are blunt instruments. They save money, yes, but they also create gaps in care. The real solution isn’t more rules. It’s better data, clearer formularies, and fairer reimbursement. Until then, patients and providers need to stay informed, ask questions, and push back when coverage gets in the way of health.
Timothy Haroutunian
February 20, 2026 AT 18:32The sheer inconsistency across states is absurd. One person in Colorado spends six months jumping through hoops just to get a generic blood pressure med, while someone in Vermont walks in and gets it for free with no questions asked. This isn't healthcare-it's a bureaucratic obstacle course designed by people who've never had to choose between food and medication. And don't get me started on the pharmacy benefit managers pulling strings behind the scenes. They're not saving money-they're gaming the system to maximize profits while patients suffer.
I’ve seen this firsthand. My cousin has type 1 diabetes and was denied a generic insulin because her state’s formulary only covered one brand. She had to switch to a different insulin, which caused severe hypoglycemic episodes. Took three appeals, two doctor letters, and a month of panic before they relented. All because some spreadsheet in Austin decided which generics were 'preferred' based on rebate deals, not clinical outcomes.
And yet, no one talks about this. The media focuses on brand-name drug prices, but the real horror is in the generics-the ones we assume are safe, cheap, and universally available. They’re not. They’re weapons in a cost-cutting war waged on the most vulnerable. We need federal standardization. Not more state-by-state patchwork. That’s not policy. That’s negligence.
Erin Pinheiro
February 20, 2026 AT 21:37i hate how states just make up rules like its a game of monopoly. like why does texas charge 5 bucks for one generic and 1 for another when theyre the exact same chemically?? its so stupid. and dont even get me started on prior auth. my mom had to wait 3 days for a simple blood pressure med because some guy in a cubicle in ohio had to 'review' it. she missed her dose and ended up in the er. its not healthcare its a nightmare.